Integrated Health Scholars Program

Program Purpose
We aim to increase the supply of social work professionals prepared to provide high-quality integrated health services in rural Federally Qualified Health Centers (FQHCs) throughout Kansas.
Program Overview
Each year, we support 12 Scholars who:
- Receive a $25,000 scholarship during their clinical specialization year
- Participate in monthly value-added training in integrated care
- Complete a rural FQHC practicum with a Capstone project
- Commit to post-graduation work in a rural community
Eligibility & Selection
We are now accepting applications for 2026-27 Integrated Health Scholars!
Eligibility Requirements
Requirements to apply for the Integrated Health Scholars Program:
- Be a current foundation year KU MSW student in good standing or an incoming advanced standing student/applicant beginning a clinical practicum in fall 2026
- Reside in rural Kansas (or have obtained clinical practicum placement in rural KS)
- Per federal guidelines, must be U.S. citizen or permanent resident
- Work with the Practicum Office to successfully secure a qualifying Integrated Health Scholar's practicum.* Please note that IHSP practicums are limited.
*The primary goal of the Scholars Program is to increase the number of social workers providing integrated care services in rural Federally Qualified Health Center (FQHCs) in Kansas. Accordingly, we prioritize placing Scholars in practicum settings at rural FQHCs (see Practicum Partners below).
However, students placed in other rural Kansas integrated care settings – such as Certified Community Behavioral Health Centers or hospitals – may also be eligible. Applicants to the Scholars Program will work closely with the Practicum Office, which is responsible for matching students with eligible practicum placements. The IHSP does not coordinate or assign students’ practicum placements.
Application and Selection
Complete the online application, including a current resume and letter of recommendation.
For a preview of application questions and recommendation instructions: IHSP Application Preview (.pdf).
Deadline for priority consideration is February 20, 2026. Applications that move forward in the process will be invited to interview with the selection committee.
Approximately 12 Scholars will be selected each year.
Virtual info sessions will be held:
- Wednesday, January 28, 2026, from 12-1 pm (register for Jan. 28 info session)
- Friday, February 6, 2026, from 12-1 pm (register for Feb. 6 info session)
Practicum Partners
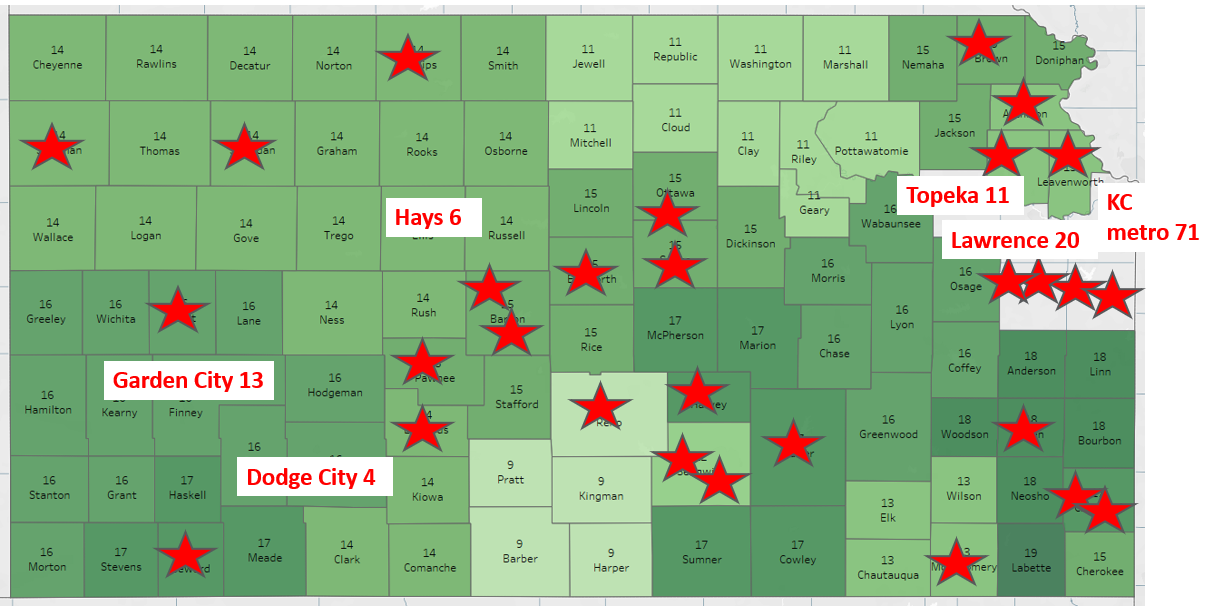
Practicum sites for Scholars are Kansas FQHCs that provide opportunities to experience working in integrated health, providing team-based care within high-need rural communities.
What are FQHCs?
Federally Qualified Health Centers (FQHCs) are community-based health providers that offer comprehensive primary, behavioral and preventive care to underserved populations, regardless of ability to pay. Many also provide dental, pharmacy, and supports for non-medical needs. Kansas has 22 FQHC systems with about 175 sites, including community, migrant, homeless, school-based, and "look-alike" clinics.
FQHC practicum partners include:
- Community Health Center of Southeast Kansas
- Genesis Family Health (Garden City & Dodge City)
- Greeley County Health Services (Tribune)
- Health Ministries Clinic (Newton)
- Heart of Kansas Family Health Care (Great Bend)
- Konza Prairie Community Health Center (Junction City & Manhattan)
- PrairieStar Health Center (Hutchinson)
- Salina Family Healthcare
- and more!
Learn More about Integrated Care
Social Workers in Integrated Health Care
The Scholars
Integrated Health Scholars
View the Capstone Project posters here
Maddie Backus - Bert Nash Community Mental Health Center (Lawrence)
Manualizing Anxiety Groups for Consistent and Trauma-informed Service Delivery - This project aims to improve service delivery for clients who utilize anxiety group therapy services at Bert Nash Community Mental Health Center by addressing consistency and trauma informed care. This project was accomplished through collaboration with center clinicians and other student interns. The goal of this project was to develop a manual for anxiety group that acts as a reference for and catalogue of group therapy intervention strategies. The strategies are organized using a CBT framework. This project addresses trauma informed care by updating group rules to meet the needs of the center's client population. This manual will allow other clinicians to cover the group with less disruption to clients while also reducing burdens on the clinician to identify appropriate and effective interventions when providing coverage.
Christina Bloomquist - Bert Nash Community Mental Health Center (Lawrence)
Tobacco Cessation: Resources for Accessibility and Affordability - This project consisted of research and discussion with interdisciplinary professionals to address accessibility and affordability barriers to tobacco cessation for low-income clients that the agency serves. The result is that there needs to be further education and training to increase awareness and offer strategies for how to navigate through these barriers to improve tobacco cessation and access to resources to improve the overall wellness of our clients that we serve within the community. Tobacco prevention and tobacco cessation impacts both mental health and the physical health of the individual, which can leads to reduced health risks and longer life expectancy for the participant.
Lorena Brooks - Johnson County Adult Therapeutic Community (Olathe)
Therapeutic Alliance: Building Relationships to Enhance Treatment Outcomes In Substance Use Disorders - Therapeutic Alliance- Building Relationships examined factors that create strong alliances between clients and their Substance Abuse Counselors (SAC) during treatment. The TC clients took the Working Alliance Inventory Short Revised (WAI-SR) survey to measure their current alliance with their SAC in the TC program. Research shows that establishing an early alliance is a consistent predictor of greater treatment outcomes. The TC clients expressed a level of comfort that has helped them work with their SAC to build the skills that they need and will help them throughout recovery.
Aubree Bryan - Munson Army Health Center - Corrections (Leavenworth)
Grief Behind Bars - Grief Behind Bars was created to help incarcerated individuals navigate grief they may experience while confined, while also giving them tools to heal. The United States Disciplinary Barracks offers multiple classes and workshops to help their incarcerated population, yet none of them are geared toward grief. My six-week course is an attempt to try and fill a need that can often be overlooked within the confinement setting.
Adam Byrd - The Guidance Center (Leavenworth)
Shining a Light on Recovery: Drug Court A Beacon Navigating towards Hope - This project intended to educate Leavenworth County decision makers on the benefits of adopting a drug court. Leavenworth County lacks sufficient means to provide accountability and alternatives to incarceration for those who live with substance use disorders. As an option to incarceration, drug courts reduce the burden and costs of repeatedly prosecuting low-level, non-violent offenders through the court system, while providing offenders an opportunity to receive treatment and education. This proposal allows Leavenworth County the ability to increase the percentage of addicted offenders to achieve sustained recovery, improving public safety and reducing the cost associated with re-arrest and additional incarceration. The drug court model integrates community resources to provide a more holistic, wrap-around support system aimed at addressing underlying trauma while promoting resilience in those that participate.
Jordan Claeys - Bert Nash Treatment and Recovery Center (Lawrence)
Means Reduction: Preventing Suicide through Time-based Prevention - The Treatment and Recovery Center (TRC) is 24/7 a crisis center aimed at serving clients in need of short-term intervention. A large population of the clients served endorse suicidal ideation in the past or currently, and have identified methods of how they would act. Due to crises being time-sensitive, creating barriers to these methods can help save a life. Providing locking bags to clients at the TRC supports time-based prevention, focusing on the immediate access to lethal means to prevent suicide.
Clayton Cook - Community Health Center of Southeast Kansas (Pittsburg)
Grief Support and Education in Rural Kansas - This project's goal was to address gaps in my rural community's access to quality mental health care related to grief and loss. These gaps were identified as a lack of community support and room for improvement in providers' knowledge of current grief best practices. The first gap was addressed through the creation of a grief support group open to all community members that met monthly. The second gap was remedied through surveying community mental health providers' understanding of approaches to grief and providing education where there were deficits.
William Crankshaw - HealthSource Integrated Solutions (statewide)
Follow-up for 988 Lifeline- A collaborative effort between 988 Suicide & Crisis Lifeline phone, chat, and text contacts, through HealthSource Integrated Solutions affords individuals anonymity, unless they wish to participate in follow-up. When an individual reaches out to 988, this may be the first experience with anyone in the mental health field. When follow-up occurs, it provides the client an opportunity to determine what their needs are, while giving a Crisis Counselor the possibility to reassess, determine if further follow up is needed, and collaborate with a client in providing provide referral to other resources.
Virginia De La Rosa - Stormont-Vail Health Systems (Topeka)
From Hospital to Home: Addressing Barriers to Safe & Equitable Discharge - This project examines the barriers to effective discharge planning through the perspectives of hospital social workers and case managers. By identifying systemic and patient-level challenges, the study proposes an evidence-informed follow-up program designed to enhance continuity of care and reduce readmissions. Although the proposed pilot program has not yet been implemented, its framework offers a foundation for improving hospital discharge processes through an integrated, person-centered approach. Additionally, this project aligns with the former Multi-Visit Program, leveraging existing resources to improve patient support post-discharge.
Marcello Dodd-Holliday - Central Kansas Mental Health Center (Salina)
Breaking the Stigma, Building Resilience - My practicum provided an opportunity to be involved in a pilot program supporting college students with mental health needs. This project explored the stigma surrounding mental health in college students and their comfort level in expressing mental health challenges. It raised awareness, encouraging students to recognize that their feelings and emotions are valid. Most importantly, it emphasized the availability of safe spaces where they can be seen, heard, and supported.
Sarahpheena Henry - Children's Mercy DAY Clinic (Kansas City)
Promoting the Use of Teen Group Therapy - This project explores the promotion and implementation of group therapy for metro area teens experiencing anxiety and depression. With youth mental health issues on the rise, there is a pressing need for therapeutic approaches that are both effective and accessible. This project supports Teen Group Cognitive Behavioral Therapy as a clinically validated, cost-effective alternative to individual therapy. Two teen specific group therapy programs were introduced at Children's Mercy's DAY Clinic, leading to reported improvements in emotional regulation and peer connection among participants. The findings emphasize that group therapy not only meets clinical needs but also addresses systemic barriers to care access, making it a valuable model for youth-serving agencies.
India Herman - Community Children's Center (Lawrence)
Expanding Services through Collaborative Relationships - This project seeks to expand the Family Resource Center (FRC)’s services by strengthening partnerships with local healthcare providers, schools, and community agencies to create an integrated support system. Through these connections, we aim to reduce barriers to care, increase awareness of available services, and ensure families can easily access the support they need. Our goal is to build a more cohesive community network that enhances family well-being and fosters meaningful collaboration across agencies.
George Kircher - Bert Nash - Douglas County Jail (Lawrence)
Mobile Competency Restoration - This project outlines the functionality, impact, and significance of Mobile Competency Restoration. The demand for inpatient hospital beds has drastically exceeded their availability, resulting in a wait time of up to 14 months in the county jail. This program was initiated to allow lower-risk defendants to complete their restoration in the Douglas County Jail, thereby facilitating quicker courtroom proceedings and reducing waiting times in jail. Through my project, I aimed to gain a deeper understanding of this program by evaluating its impact, with the goal of educating my peers and community.
Caitlynn McClellan - Mosaic Life Care at St. Joseph Medical Center (St. Joseph)
Enhancing Accessibility and Bridging Language Barriers: Implementing In-Person Chuukese Language Translators - This proposal aims to implement in-person Chuukese language translators within the organization of Mosaic Life Care hospital and its clinics. This would improve accessibility for the demographic of individuals in this community who speak Chuukese, eliminating language barriers effecting equal access to services and care, and promoting inclusivity, understanding, and support for the needs of the Chuukese community. This aligns with the organization’s mission to improve population health outcomes in our region by providing the right care, at the right time, place and cost.
Jerry McKay - University of Kansas Medical Center - Trauma (Kansas City)
The Microcosm of Secondary or Vicarious Trauma in Intensive Care & Inpatient Trauma Departments - Clinicians working in hospital settings are routinely exposed to the physical, psychological, and emotional burdens of their patients, placing them at a significantly greater risk for secondary traumatic stress (STS). Despite the awareness, the subtle and often underrated nature of this occupational hazard and ongoing exposures remain insufficiently addressed in both research and institutional practice. This comprehensive overview examines the high-risk factors contributing to STS. Using evidence-based screening tools such as the Secondary Traumatic Stress Scale (STSS) and strategies to mitigate these risks with trauma-informed practices, we can foster psychological safety and cultivate a culture of empathy.
Chloe Meisel - Children's Mercy Acute Mental Health Screening (Kansas City)
Acute Crisis Intervention: Evaluating Treatment Modalities in Youth Psychiatric Facilities - This project aims to help reduce the rates of revisits to the Emergency Department for youth on the basis of mental health by evaluating the effectiveness of treatment modalities utilized in youth inpatient psychiatric care and working toward universal implementation of effective strategies. The goal is to better understand how we can effectively support youth in mental health crises to prevent readmission both in the Emergency Department and in acute psychiatric care facilities, as well as promote supportive aftercare following discharge from acute stays and target barriers to types of preventative support needed for youth mental health care.
Jillian Mitchell – The University of Kansas Cancer Center – Olathe Campus (Olathe)
Caregiving through Cancer: The Role of Oncology Social Workers in Supporting Parents and Primary Caregivers with Their Own Cancer Diagnosis - A cancer diagnosis and subsequent treatment can exacerbate the stress that parents and guardians experience. Caregivers must care for their own upended social, emotional, and physical health while also supporting their children through this time of uncertainty. This project aims to provide support for caregivers with minor children by providing education, connections, and resources to caregivers while also providing a guide for social workers to use as they work with caregivers.
Natalee Morris - Mercy Hospital (Pittsburg)
Social Workers Contributing to Healthcare Literacy - This project was utilized to collect information on various aspects of healthcare. Some categories included health insurance types and coverage, local food assistance, and home services for the elderly population. This information was then compiled into one document that can be shared with students, clients, and new workers as a starting point for health care information sharing in an acute care setting.
Callie Nichols - University of Kansas Health System – Continuum of Care, MVP Program (Kansas City)
Improving Diabetes Care: A Social Work Assessment Tool for Multi-Visit Patients - This project developed a diabetes-specific assessment tool for social workers in the Multi-Visit Patient (MVP) Program at The University of Kansas Health System. With diabetes being a common diagnosis among MVPs, this tool helps identify social, emotional, and practical barriers to self-management. By incorporating targeted questions on diabetes management, this tool helps provide more person-centered, comprehensive care.
Abigail Okesanya - Valeo Behavioral Health Care (Topeka)
Exploring Factors behind Readmission to Outpatient Psychotherapy: Why Clients Return after Discharge - Understanding why clients are readmitted to outpatient psychotherapy services (OPS) after discharge is critical for improving mental health outcomes and supporting clients in maintaining independent coping strategies. Qualitative survey data was collected from both clients and psychotherapists to investigate factors that contribute to readmission for OPS at Valeo. Results reinforce (1) the need for a healthy therapeutic relationship, (2) the benefits of discussing intervention rationale, and (3) the value of implementing a pre-discharge structure that encourages clients to practice independent coping prior to their final session to better anticipate potential barriers and inform clinician efforts to prepare clients for successful discharge. Project conclusions will inform departmental strategies for effective discharge planning.
Clair Perry – Children’s Mercy Primary Care Clinics (Kansas City)
Primary Care Supervisory Training for Dependently Licensed Social Workers - This project advocates for the implementation of a fellowship program to train social workers as behavioral health clinicians (BHCs) in integrated behavioral health (IBH) programs within the Children’s Mercy Primary Care Clinics. By addressing systemic inequities, reducing emergency department utilization, and improving access for underserved populations, IBH programs enhance outcomes for children and families. Social workers bring unique expertise in systems theory and culturally responsive care, making them integral to these models. Additionally, the project highlights practical skills gained through IBH training, such as interventions for excoriation, pica, pill swallowing, and delayed toilet training, demonstrating the value of interdisciplinary collaboration at Children’s Mercy.
Vera Petrovic - Bert Nash Mental Health Center (Lawrence)
“Navigating Obsessive-Compulsive Disorder”: Filling Service Gaps through Group Therapy - The Bert Nash Center, which serves residents of Douglas County and beyond, maintains a variety of group therapy options intended to facilitate peer-learning and bolster community-building. However, of the approximately 20 groups offered within the Adult Outpatient Program (AOP) as of August 2024, none addressed the treatment of obsessive-compulsive disorder (OCD). In an effort to fill this service gap, this project involved the design and implementation of a weekly OCD psychoeducation/skills group. Drawing from the work of Jonathan Grayson and other OCD experts, the program sought to provide an accessible, welcoming space in which clients could learn about their diagnosis, connect with others, and develop a range of skills and coping strategies to help manage distressing symptoms.
Kiersten Rogers - Salina Family Healthcare Center (Salina)
Youth Mental Health Resources and Suicide Awareness - Youth mental health is often hidden behind closed doors, putting youth at a greater risk. Due to stigma around mental health, parents and caregivers are often left in the dark and become quickly overwhelmed when faced with their child struggling with mental health or expressing suicidal ideation. The goal of my project is to make this information easily accessible in a pamphlet that caregivers can read over and refer to as needed so they can recognize signs that their child may be struggling, be aware of resources locally and nationally to get them help, and know what to do if their child becomes suicidal. The pamphlet also provides information for caregivers struggling to cope with helping their child with mental health, and statistics about youth mental health to help educate caregivers.
DaiJa Scruggs -Saint Luke's Hospital (Kansas City)
The Impact of Patient Deaths on Healthcare Workers - This project explores the impact of patient deaths on healthcare workers, a critical yet often overlooked aspect of their mental health. While death is a natural part of life, repeatedly witnessing it in a short period is not, making it difficult for healthcare workers to process their grief. Without proper support, many develop compassion fatigue or emotional numbness as a coping mechanism. Implementing strong support systems, effective coping strategies, and specialized training can help mitigate these effects. Social workers play a vital role in this process by providing emotional support and advocacy for their fellow healthcare team members.
Lena Shelton – Family Service & Guidance Center (Topeka)
Expanding Treatment Accessibility through In-house Free Childcare - This project sets out to bridge a gap in accessibility at Family Services and Guidance and increase session attendance as well as increase focus within session. Exploring the potential for free, short-term childcare for parents and families while they attend their scheduled sessions would open the door for the needs of those with young children to be met.
Amanda Van Tuyl – Saint Luke’s Abdominal Transplant (Kansas City)
Kidney Transplant Health Literacy Documents & Screening - Understanding medical conditions and terminology can be challenging, especially for patients going through the transplant process. This process is complex and time consuming, and often these individuals feel ill and exhausted, making it harder to comprehend critical medical information. The implementation of the KTUT screening tool, along with the creation of the scoring guide and health literacy documents, will simplify these complexities. By presenting information at the patient's comprehension level, these tools enhance understanding and ultimately improve health outcomes.
Jaclyn Wilburn – KU Alzheimer’s Disease Research Center (Fairway)
Hooray for the Bidet! Introducing an Affordable and Functional Tool with Broad Applications in Patient Care - Individuals with cognitive impairment and/or their care partners can be physically and emotionally exhausted by performing Activities of Daily Living (ADLs). This project introduces the bidet attachment as a practical and affordable household tool that will promote the dignity and worth of the person with the disease. The Hooray for the Bidet Guide showcases the bidet attachment as an affordable and functional resource that can benefit people of all ages and abilities, not just those with cognitive impairment.
LaShea Young - Wyandot Center PACES (Kansas City)
Mental Health for Kids and Teens with Diabetes - This project advocates for an integrated healthcare approach to address the physical and mental health needs of minority youth with diabetes in low-income communities. It emphasizes the importance of routine mental health screenings, multidisciplinary care, and the pivotal role of social workers using frameworks like Ecological Systems Theory and Strengths-Based Approach. This initiative highlights Certified Community Behavioral Health Clinics (CCBHCs) as key providers of comprehensive, community-based services that combine diabetes and mental health management, aiming to reduce health disparities and improve outcomes for underserved youth.
View the Capstone Project posters here
Sarah Barth - A Connecting Pointe (Olathe)
Identifying Gaps in Suicide Prevention in Adult Treatment Courts - A Connecting Pointe partners with Johnson County's Adult Drug Court to provide therapeutic services for individuals suffering from substance use disorders. The goal of this project was to identify gaps in intervention and assessment services and to increase understanding of team members' awareness of and comfort in discussing suicide risk with clients. I created a survey and invited all Drug Court team members and A Connecting Pointe staff to participate. Survey outcomes were analyzed to determine the team's strengths and key points for intervention.
Brooke Benton - Research Psychiatric Hospital (Kansas City, MO)
Patients’ Perceptions of Trauma Informed Care - This project sought to quantitatively and qualitatively analyze patients’ perceptions of the implementation of Trauma-Informed Care (TIC) practices within an adult inpatient psychiatric hospital. This was accomplished by administering the mixed methods Trauma-Informed Care- Client Feedback Survey (CFS) published by The National Council for Behavioral Health and performing a qualitative content analysis for the open-ended question embedded in the CFS. Results indicated both strengths and areas of improvement. Future recommendations to accomplish increased TIC practices within a psychiatric inpatient setting, and across multiple disciplines, can be implemented on both organizational and clinical levels.
Kareesha Boyington - Preferred Family Healthcare (Joplin)
Bridging the Gap: Substance Abuse Services Before a Juvenile Officer - Within my practicum over the past year, I have consistently listened to the staff outline the gap in services seen for adolescents who could benefit from substance abuse services but do not have a juvenile officer to refer them. Working in collaboration with the local high school, I set out to create a connection between the two agencies and place brochures and information guides within the building. Through these efforts, we can begin to fill this gap and spread information to the targeted population about potential services before it gets to the point of requiring a juvenile officer.
Sydnee Bradley - Kansas Suicide Prevention HQ (Lawrence)
Bridging the Gap in Rural Suicide Prevention: Barriers to Consider When Approaching Men and Farmers in Rural Communities - Incoming phone call contacts on the 988 suicide prevention lifeline through Headquarters Kansas showed a gap in accessibility of care for men struggling with suicidal tendencies and mental health crises. Suicide death rates are rising each year in Kansas and the population with the highest rate of death by suicide are adult men. Rural counties often lack adequate prevention and intervention for suicide due to barriers such as stigma, agricultural values being invalidated, and lack of access to healthcare and mental healthcare. This project explored research on what men and male farmers share to be barriers to mental health care and suicide prevention efforts, as well as research-based applications shown to help remove those barriers.
Destinee Brown - Camber Children’s Mental Health- KC (Kansas City, KS)
Life After Discharge for Youth Admitted into Mental Health Hospitals - This project intended to educate guardians on the heightened risk that discharge from a psychiatric setting has on client’s health and inform them of the importance of guidance, support, and therapeutic assistance during this stage of the clients’ lives. Hospital settings provide structure and safety which may not be as accessible to clients post discharge thereby increasing their sense of vulnerability and use of maladaptive coping skills. Research shows that psychiatric discharge is linked with increased risk, trauma, ideations, and self-harm behaviors. Since post discharge is a risky period for clients, it is essential that they seek services immediately after discharge for continuity of care, future health and well-being.
Brittany Burgess - Bert Nash Mental Health Center (Lawrence)
Crisis Intervention and Barriers to Recovery - The Treatment and Recovery Center (TRC) is a 24/7 crisis center which provides short-term crisis intervention and stabilization services and is a collaborative effort between Douglas County and Bert Nash Mental Health Center. Because of the complicated nature of crises, some clients return to the TRC multiple times for assistance. Data for the top 20 clients with the most return visits in a six-month period was analyzed and compared to the rest of the client population. The aim of this project was to gain insight into this population and begin identifying common barriers to their ability to recover from crises.
Marisa Butler - ReStart, Inc. (Kansas City, MO)
Service Delivery to the Unhoused: A Community Needs Assessment - Interviews were conducted with ReStart residents on the current services they were receiving, ease of access, as well as needs they had that were not being met. A final question was asked about what programs they could envision that would better serve their needs. Community leaders serving the unhoused population of Kansas City were also interviewed on the programming they offered, changes over the years, as well as unmet needs and visioning of ideal programming. Data will be shared within ReStart to assist with program evaluation and development as well as centering client needs and experiences. In the future, a larger survey could be conducted across a variety of agencies to give a more comprehensive snapshot of the needs of this community with findings used as an advocacy tool for improving services.
Bertha Covarrubias - Vibrant Health (Kansas City, KS)
Bienvenido: La Buena Salud Emocional para el Inmigrante: Good Emotional Health for the Immigrant - Vibrant Health is a community-based clinic that offers medical, dental, behavioral health, women’s health and pharmacy services. Vibrant provides services on a sliding fee scale, offers extended hours and has a diverse group of providers and staff that seek to reflect the community that it serves. Currently, Vibrant Health has a large percentage of patients that prefer services in Spanish. With the growing population of newcomers from Latin American countries the program “Bienvenido” was a perfect fit for Vibrant to offer support to these patients. This program focuses on mental health topics, education regarding substance misuse and how it relates to Latino immigrants.
Irvin Garcia-Augur - Crawford County Mental Health Center (Pittsburg)
SBIRT – Screening, Brief Intervention and Referral to Treatment - The SBIRT project is a brief intervention model that is evidence-based and similar to routine checkups to help clients reduce or abstain from substance use. Crawford County Mental Health Center serves clients who are not ready to quit substance use, but that is the beauty of SBIRT. This intervention works at the client's pace by using motivational interviewing techniques, which empowers the client to make changes themselves.
Maddi Gilliam - Grand Falls Center for Recovery (Joplin, MO)
Joplin, Mo Free Public Transportation (with Alaina Morgan – Ozark Center) - There is a lack of free public transportation in Joplin, MO. Joplin has not had free transportation since November of 2022 due to a shortage of drivers. This provides barriers for people trying to receive mental health and substance use services. The changes we propose are for Joplin Public Works to partner with Economic Security CARS (Community Action Ride System) program and allow people to volunteer to drive the trolley.
Lauri Goheen - Salina Family Healthcare Center (Salina)
Enhancing Behavioral Healthcare at FQHCs: Collaboration and Innovations -Projects at Salina Family Healthcare Center (SFHC) aimed to enhance behavioral healthcare delivery through collaborative efforts, emphasizing the role of social work in promoting community well-being. Innovative approaches and interprofessional collaboration were central to improving access to services, reducing stigma, and fostering holistic care. Key initiatives included integrating teletherapy services, expanding students' clinical experiences under social work supervision, and advancing person-centered care approaches tailored to the community's diverse needs.
Jennie Gusewelle - KU Alzheimer’s Disease Research Center (Fairway)
Understanding Your Options: Home vs Community Living as You Age - Deciding whether to remain at home or move into a community as one ages can be difficult. This decision is often made more difficult by not understanding how much or if health insurance will cover the cost of future needs. The goal of my project is to empower older adults in making this decision by creating a guide to understanding their options. It will be a booklet that patients can take with them presenting an overview of Medicare, Medicaid and Veterans benefits related to care in the home and in community settings. There also will be descriptions of different types of residential communities. And it will include some of the benefits and drawbacks of either living at home or joining a community, as well as strategies for making each successful.
Kristene Hampton - Wyandot Center – Adult Outpatient (Kansas City, KS)
Trauma-informed Expressive Group Therapy - Expressive therapy has many benefits beyond improving well-being. Expressive therapy also has cognitive benefits, including helping those who have experienced trauma make sense of their experiences. Through various methods, including painting, music, and writing, individuals may explore their experiences using nonverbal outlets. Creatively expressing emotions through the medium of art helps those with trauma gain insight into their experiences in a safe, supportive environment, fostering a sense of empowerment and healing.
Braeden Hinton - Crawford County Mental Health Center (Pittsburg)
ADA Accessibility - My Capstone Project included an in-depth look at our agency buildings and their accessibility to services for those who have a physical disability. I was able to use Americans with Disabilities Act (ADA) tools provided by my agency, as well as volunteers that have physical disabilities to conduct this survey of our agency. With the addition of this survey, Crawford County Mental Health Center meets ADA requirements to further their advancement into becoming a Certified Community Behavioral Health Clinic (CCBHC) and makes their services accessible to every individual.
Athena Horton - Camber Children’s Mental Health- KC (Kansas City, KS)
The Development of a Sensory Space in a Children’s PRTF - This project addresses the need for additional support for a specialized population at Camber Children's Mental Health PRTF. Residents with Intellectual and Developmental Disabilities (I/DD) face challenges with sensory modulation, often leading to disruptive externalizing behaviors. Sensory spaces offer tools that promote effective sensory processing, provide avenues for de-escalation, and ultimately reduce rates of utilizing restraint and seclusion as an intervention.
Gabriel Hurtado - Arista Recovery (Paola & Overland Park)
The Recovery Gap: Urban and Rural - Nationally and locally, there has been a steady increase and growing awareness in the need for more integral, holistic treatment centers for substance use disorders (SUD). To better reach, inform, empower, and eliminate stigma related to recovery, my project involved collecting data from Arista’s treatment centers in Paola and Kansas City and exploring client-level barriers and themes related to accessing treatment, during and after outpatient. Challenges varied between rural and urban with common themes including a shortage of sustainable holistic-person-centered treatment options and stigma. While work is needed in general to address access gaps, Arista is actively seeking solutions in both holistic and integral realms.
Aliya Jankowski - Bert Nash WRAP Program (Lawrence)
Designing with the Community in Mind - There is a large gap in the youth crisis continuum in Lawrence-Douglas County. Although the Treatment and Recovery Center (TRC) offers urgent care, continued observation and stabilization of youth often occurs in other counties. The Youth Recovery Center (YRC) aims to fill this gap, and including community input in its design will be critical to its success.
Ashley Keller - BlueStem PACE (Hutchinson)
Behavioral Health Leveling for Integrated Care - As an all-inclusive care provider, the need for a standardized structure for responsible interdisciplinary care planning was identified. A leveling system was developed to allow the interdisciplinary team “at-a-glance" information on behavioral health data important for providing health care. Mental health diagnoses, medications, behavioral health histories, and relevant ongoing assessment information was collected and displayed on a shared spreadsheet to reference in the care planning process. This system improved reliability of equitable access to healthcare for participants with behavioral health needs.
Sophia Kenney-Tolentino - Pawnee Mental Health Services (Manhattan)
Improving Intra-Agency Communication - Effective intra-agency communication is essential for robust continuity of care for all clients. For Pawnee Mental Health Services, a Community Behavioral Health Clinic (CCBHC) serving 10 counties in northeast Kansas, there was no centrally accessible internal directory of the programs offered by the agency, leading to gaps in communication among staff and potentially in services. I worked with agency administration and leadership teams to gather detailed information on all Pawnee programs, then compiled it into one document to be added to a central location for all staff across the state to access. Interprofessional communication is a fundamental piece of integrated mental health care and when all staff are knowledgeable of the services an agency provides, fewer clients will fall through the cracks.
Adam King - Four County Mental Health Center (Independence)
Assessing Trauma-informed Care Practices with Certified Community Behavioral Health Centers and their Community Partners - In the realm of community behavioral health, ensuring trauma-informed care practices are paramount for effective service delivery. This project focuses on assessing such practices within Four County Mental Health Center in Independence Kansas, a Certified Community Behavioral Health Clinic (CCBHC) and their community partners. By employing a comprehensive evaluation framework, including surveys, interviews, and observational assessments, this study aims to illuminate the strengths and areas for improvement in trauma-informed care provision. Through collaboration with diverse stakeholders, including clinicians, administrators, and clients, insights will be gathered to inform targeted interventions and policy recommendations. Ultimately, the goal of this project is to enhance the quality and accessibility of trauma-informed care, thereby fostering resilience and well-being within communities served by CCBHCs and their partners.
Anna Kostecki - Children’s Mercy (Kansas City, MO)
Emergency Department Environments & the Trauma-informed Use of Restraints -The Acute Mental Health Screening Team (AMHS) at Children’s Mercy Hospital (CMH) plays a crucial role in assessing and serving children and families in acute mental health crises presenting to the Emergency Department. This project aims to evaluate the functionality of the AMHS environment and examine the impact of trauma-informed care on reducing unnecessary restraints. Through an evidence-based assessment process, patients presenting with suicidal ideation, homicidal ideation, behavioral complaints, or other mental health needs receive appropriate disposition, such as inpatient psychiatric admission or connection with outpatient resources. By analyzing data metrics and exploring the integration of trauma-informed practices, this project seeks to enhance patient outcomes and optimize resource utilization within AMHS at CMH.
Diana Lady - Elizabeth Layton Center (Ottawa)
Implementing Trauma-informed Care- This project outlines the journey of implementing Trauma-Informed Care (TIC) practices at Elizabeth Layton Center (ELC), an outpatient mental health provider seeking certification as a Certified Community Behavioral Health Clinic (CCBHC). Beginning with a review of existing TIC practices prompted ELC to proactively identify areas for improvement. Conceptualizing a workplace wellness room to promote mindfulness and relaxation for mental health practitioners and administrative staff reflects ELC's commitment to staff well-being. This work emphasizes the significance of addressing trauma within the workplace, underscoring the holistic person-centered approach of TIC and its impact on individual well-being and organizational effectiveness thereby showcasing ELC’s dedication to providing supportive services and prioritizing the well-being and resilience of both clients and staff members.
Cooper Mickelson - Valeo Outpatient (Topeka)
Facilitating Communication in Integrated Care Settings - Communication is crucial in integrated health settings. Reliable lines of communication between the myriad of professionals working on an individual’s treatment team helps to increase the quality of care. Unfortunately, healthcare, even in many integrated settings, remains siloed. This inhibits a holistic treatment approach and negatively impacts care efficacy. This project explores the importance of communication in integrated care and draws upon information gained from interviews with executive and organizational leadership to analyze barriers to effective communication as well as postulate potential solutions to current communication deficits.
Alaina Morgan - Ozark Center - New Directions (Joplin)
Joplin, Mo Free Public Transportation (with Maddi Gilliam – Grand Falls Center for Recovery) - There is a lack of free public transportation in Joplin, MO. Joplin has not had free transportation since November of 2022 due to a shortage of drivers. This provides barriers for people trying to receive mental health and substance use services. The changes we propose are for Joplin Public Works to partner with Economic Security CARS (Community Action Ride System) program and allow people to volunteer to drive the trolley.
Sophia Nangia - Johnson County Adult Therapeutic Community (Olathe)
Life Beyond TC - At the Johnson County Adult Therapeutic Community (TC), outcomes of released clients are not evaluated and there are no post-release check-ins. It is valuable to have outcome data on clients who leave a program. This project conducted a qualitative study interviewing released clients. The purpose of gathering data was to understand life after TC. Specifically, I wanted to know some of the common outcomes and struggles clients face once released as well as how TC could do more to help future clients.
Mary Catherine Newman - KU Alzheimer’s Disease Research Center (Fairway)
Common Grounds - Caregiving for a loved one living with Alzheimer’s or dementia is a unique journey that's known to many. Informally connecting with others in community settings offers both accessibility and normalcy around a diagnosis that has the potential to isolate caregivers. From small towns to bustling cities, creating a regular touchpoint is both doable and essential for the well-being of both the caregiver and the patient depending upon a reserve of strength, hope, and love.
Alex Scott - Johnson County Mental Health Center (Overland Park)
Gun Store Suicide Prevention Outreach - After identifying around 150 gun dealers in Johnson County, in-person outreach took place at over a dozen pawn shops, big box stores, and brick-and- mortar gun shops. We provided education and uniquely designed suicide prevention resources such as gun locks with the suicide prevention hotline number, specially designed 988 cards to be given away with newly purchased firearms, and suicide prevention posters. A specialized brief suicide intervention training was held in early April 2024 for gun store staff.
Lauren Stiles - Community Health Center of Southeast Kansas (Pittsburg clinic)
New Employee/Intern Orientation Manual - To be a functioning and productive member of a mental health team requires intimate understanding of policies and workflows. Not only is an adequate understanding of many of these aspects a legal requirement in many cases, but it also serves as the groundwork for a functional work environment that is not only safe, but effective and looking out for both its patients’ and employees’ wellbeing. This project aims to put all of those policies in one place in a succinct and easy to follow manner.
Mimi Tomay-Trinidad - Crawford County Mental Health Center (Pittsburg)
Medical Conditions Education in Mental Health Services - This project focused on educating therapists and case managers on medical conditions including hypertension, diabetes, asthma, tuberculosis, sexually transmitted infections, and smoking. Often clients who struggle with medical conditions also struggle with their mental health. By having mental health center staff informed on how these medical conditions can affect clients both medically and mentally, they can better serve clients through mental health services and evidence-based interventions.
Ann Wolfe - CJR 1 School District (Carl Junction, MO)
CJ Cares: Healthy Kids. Healthy Community. - The American Academy of Pediatrics selected Carl Junction (CJ) School District as one of five districts in Missouri to participate in the Health services Assessment Tool for Schools (HATS) during the 2023-2024 school year. This assessment identified the highest ranked unmet need was improving communication to families and the community regarding services that promote student health and wellness. The “CJ Cares: Healthy Kids. Healthy Community.” initiative was developed to support integrated, interdisciplinary approaches to student health, resulting in improved communication regarding district services.
View the Capstone Project posters here
Ilexa Axelrod – Health Partnership Clinic
Evaluating Current Trauma-Informed Care Practices - This project was completed through a collaboration between National Child Traumatic Stress Network (NCTSN) representatives and Behavioral Health (BH) team at Health Partnership Clinic to assess the agency's current level of Trauma-Informed Care practices. The BH team utilized NCTSN’s no-cost Trauma-Informed Organizational Assessment (TIOA) as a trial before introducing the evaluation process to the entire agency. Outcomes revealed strengths, areas of improvement, and additional considerations.
Megan Belaire & Clara Selam – Headquarters Counseling Center
Mental Health and Mobile Response in Douglas County - Douglas County launched a Mobile Response Team (MRT) to respond to mental health crises within the county. A program evaluation of this service determined adherence to national standards and areas for growth. The Haskell Emergency Response Team (HERT) is the point of contact for Haskell Indian Nations students to report incidents and emergencies (including mental health emergencies) on Haskell’s Campus. Then they coordinate the appropriate response with one of their partners. A potential partnership between MRT and HERT could address gaps in coverage and help to enhance communication between various agencies on the crisis continuum.
Timothy Bianco – University Health Behavioral Health, Child and Adolescent Center
Increasing Awareness of Educational Resources for Children and Adolescents - This project addressed the need to increase awareness and understanding of educational-based mental health systems and resources amongst Qualified Mental Health Professionals (QMHP) and parents. The need was mitigated by the development of professional development (PD) training and organizing parent referral resources. PD training was presented to Social Work interns for constructive feedback prior to providing PD training with University Health Behavioral Health QMHPs. Parent/guardian referral resources were developed and provided to parents/guardians during initial intake assessment sessions.
Maggie Burton – Family Guidance Center for Behavioral Healthcare
Creating Group Support for Adolescents with SUD - The Family Guidance Center in St. Joseph Missouri, has recently experienced an increased demand in assistance for adolescents with substance use disorders (SUD). I assisted in developing the group type and weekly schedule for this program. The groups run Monday through Thursday from 3pm to 6:50pm. Each group runs for 50 minutes. Participants are not required to participate in all groups, but weekly engagement in at least two consistent groups is the recommendation. The group types were selected were Moral Reconation Therapy (MRT) and 12 Steps as well as educational groups to help develop skills such as relational, communication, problem-solving, and healthy coping.
Clara Chollet – MARC Head Start
Addressing Barriers within Pediatric Dental Care by Developing and Utilizing Scripted Stories - Children enrolled in MARC Head Start are eligible to receive free dental services through Swope Health’s dental bus, however, some children are unable to participate. Many children are unfamiliar with dentists and are too fearful to sit still or keep their mouths open to receive necessary dental care. A scripted story was created with detailed descriptions and pictures of every step of the process, including self-regulation strategies to support emotional well-being. Teachers will periodically read and discuss the scripted story with the children to prepare them for their dental visit to hopefully reduce instances in which a child does not receive dental care due to anxiety or fear.
Jessica Marie Pinkerton Cox – KU Medical Center Department of Pediatrics
Easing Access to Social Work in Outpatient Pediatrics - In the outpatient pediatric setting many patients are not aware of social work services and some are not able to access in-person social work at the clinic. This project consists of a website and QR code with information on social work services available to the KU pediatric patients. It will provide patients with information on what social work is and how they can access services as well as a rotating list of community resources. The project will improve the care that patients at the pediatric clinic receive by offering more equitable access to social services.
Kalisha Dixon – AIDS Project of the Ozarks
A Community In Need - Rebuilding after an epidemic is not solely based on what the epidemic directly affected but also, what the epidemic indirectly affected, for example, testing resources for those in the community potentially living with HIV/AIDS as well as other sexually transmitted infections with unmet healthcare and insurance needs. Through this process, I was able to begin rebuilding an outreach, education, and testing program based in the community and in the office in order to bridge the needs of the community to the resources that had been lost. Although this process has just begun, the relationships developed to support community needs will be life-changing, especially for the transient populations surrounding Southwest Missouri.
Cara Ebersole – University Health Truman Medical Center
Early Psychiatric Intervention and Shorter LOS - Early psychiatric intervention can lead to shorter length of stays when it comes to in patient med surge floors. Too many times we see that after 4 or 5 days of being in the hospital a patient is needing psychiatric intervention which lengthens their stay. While this is not always predictable, there are some indicators that should be considered when screening patients upon admission. For my project I used research that had already been conducted about proactive psychiatric consultation rather than reactive consultation like many hospitals follow. This allows patients with the highest psychiatric acuity to be seen sooner rather than later.
Reonna Faller – GRAND Mental Health
Child Focused Treatment Team - Oklahoma was among the first eight states selected to participate in a demonstration program of the Certified Community Behavioral Health Clinic (CCBHC) model in 2017. The program model has proven successful in improving health outcomes, access to care, reducing emergency room visits, advancing the use of Health Information Technology (HIT), and preventing unnecessary care. Integrated treatment teams are part of the CCBHC model and children’s services are among the subgroups. Understanding the different roles, responsibilities, and relationships are essential to the fidelity of the services and continuation of successful outcomes.
Chelsea Foster – GRAND Mental Health
Trauma-Informed Care for Prek-12 Educators - This project identifies the need for Trauma-Informed Care in the school system for educators. It is crucial for educators who are working with children to be trauma-informed to better understand the behaviors of children. If educators have a better understanding of trauma, effects of trauma, and how to work with children who have endured trauma they can help provide children with a safe place.
Nicole Freeman – USD 229 Blue Valley School District
School-Based Clinics in Blue Valley–Title I Elementary School - The United States struggles with identifying solutions to close the healthcare gap in low-income and rural communities. Research is proving that by implementing school-based clinics in Title I schools, overall health outcomes for students and families improve. The data collected shows that a school-based clinic in Title I schools are useful to increase students and families access to health care. There are several health partnership clinics in the state of Kansas willing to become a partner in closing the healthcare gap.
Audra Fullerton – Family Peace Initiative & Stormont Vail Emergency Department
A New Approach to Identification of and Response to Intimate Partner Violence (IPV) - Kansas has been a national leader in domestic violence offender intervention services yet these services are widely underutilized. This project highlights the current response to IPV in Shawnee County, KS, what gaps exist, and how social workers can help address the needs left by these gaps. After attending the training developed as a part of this project, 64% of attendees reported that the training had impacted their practice in a positive way (15% reported this training affirmed their current practice). Practitioners in Kansas are welcome to view the project poster and find their local battering intervention program at KS gov victim-services.
Samantha Gibson – Ascend Hospice-Lawrence
Implementing A Community-Based Support Group for Loss & Grief - Although hospice agencies that receive Medicare reimbursement are required to offer bereavement services to surviving loved ones, there is a wide variability in the types of services utilized. While completing my practicum in the Lawrence/Topeka area, I identified the need for more intensive bereavement support. Grief and mourning are highly individualized processes with significant variability culturally and socially, emphasizing the necessity of varied bereavement support services. The goal of implementing this group was to provide an additional opportunity for people to receive support and forge connection with others.
Kathryn Keyes – Lawrence Public Schools
“School-Families” Check-Ins as Intermediate Social Interventions and Positive Behavioral Supports - The impacts of home and hybrid learning during the pandemic are still being felt by all. Referrals for behavioral interventions to school behavioral health (BH) staff were higher in the 22-23 academic year. To increase support capacity, “School Family Check-Ins” were created as an immediate assessment to provide additional positive behavioral supports.
Jewel Knight – New Chance
Motivational Interviewing as a Brief Intervention for Clients with Substance Use Disorder - Motivational interviewing (MI) is an evidence-based treatment in which interviewers nurture responsibility for behavior taking steps to change. MI was the chosen treatment due ease of implementation and intervention duration (court ordered for 3 months). Of 15 clients served, 80% were first time DUI recipients, 13% relapsed, and100% of the clients completed treatment successfully.
Donald LaForte – Community Health Center of Southeast Kansas
Clinic Help for Underserved Communities and Marginalized Individuals - This project explored how marginalized and underserved populations receive care at the Community Health Center of Southeast Kansas. Personal practice experience is presented featuring diverse populations served including: lower socio-economic classes, LGBTQ+, adults who are older, foreign language speakers, hard of hearing, and houseless clients. Reflections on different ways to examine how social work can work with diverse populations is summarized.
Kira Lake – Four County Mental Health Center
Intellectual Development Disability Toolkit - Over the past year I worked as an outpatient therapist internet at Four County Mental Health Center in Cowley County, Kansas. Through my discussions with therapists, I found that a lot were seeking resources for their practice with intellectual and developmentally disabled (I/DD) clients. Throughout the past year I worked to compile a toolkit as a resource for therapists working with I/DD clients.
Chelsea Liu – Lawrence OB-GYN Specialists
Behavioral Health Integration in Perinatal Primary Care - Perinatal mood and anxiety disorders (PMADs) are highly prevalent but often go undiagnosed and untreated due to stigma, lack of information, and lack of access to perinatal mental health providers. Integrating behavioral health into perinatal care in an OB-GYN clinic is an effective way to help increase access, education, and treatment. This project highlights a pilot program in an OB-GYN clinic.
Lisa Marin – The University of Kansas Health Systems – Palliative and Hospice Services
Bridging The Language and Cultural Gap When Providing Hospice Services for Hispanic Patients and Families - Hispanic patients with Limited English Proficiency disproportionately lack access to the benefits of hospice services. An interprofessional hospice team can work together to bridge the language and cultural gap. To successfully bridge the language and cultural gap, three interventions are recommended: Cultural Humility, Culturally Informed Translation Services, and Patient Education.
Mallory Martin – Phoenix Home Care and Hospice
Suicide Ideation Amongst Hospice Patients - Discussing suicide ideation with patients on hospice services creates ethical dilemmas. Hospice social workers and chaplains need to feel competent and knowledgeable about how to navigate such conversations. A training was developed on this topic as well as an anonymous reflection survey. Results suggest increase in confidence levels after training.
Stephanie Morris – Saint Luke’s Behavioral Health- Behavioral Access Center and Psychiatric Unit
New Employee/Intern Orientation Manual - Mental health assessment and documentation is a complex and necessary process, requiring specific information and in-depth documentation. As the field changes and policies get developed, practice manuals need updating. This project summarizes the update of a “three-ring binder” in the Behavior Access Center which is now also available digitally-for the staff who work remotely, new employees, and future interns.
Emily Mushinski – Children’s Mercy
While You Wait Workshop, Addressing the Waitlist for Autism Evaluations - This While You Wait Workshop seeks to provide education and resources through a live video and PowerPoint presentation with families who have children on the waitlist for autism evaluations. This project addresses the multi-month waitlist and offers tools and suggestions for families to act on prior to their scheduled appointment.
Kristin Nichols – KUMC Alzheimer’s Disease Center
The Purpose Project at KUMC Alzheimer’s Disease Center - The Purpose Project is intended to empower individuals with Early-Stage Dementia or Mild Cognitive Impairment (MCI) to engage in purposeful and meaningful community engagement. The goal is to assist with extension of volunteerism in the community through support with non-profit organizations. This endeavor has facilitated supportive relationships and reasonable accommodations to promote participants’ increased success and confidence.
Dakota Patrick – KU Health System Care Management
Interprofessional Perspectives on the Multi-Visit Patient Program - A qualitative survey was created in collaboration with the Multi-Visit Patient (MVP) team at University of Kansas Medical Center (KUMC) to gain the insights of resident physicians in the Emergency Department (ED). The survey explores how different disciplines interact and work together toward greater patient centered care, along with role of social workers and how their role is perceived. Information from this survey will help inform education efforts by the MVP team at KUMC.
Sophie Peterson - Ascend Hospice
Adjunct Therapies in Hospice - When our loved ones enter hospice we want the best care for them. We want any service that will make their end-of-life journey comfortable and peaceful. Adjunct therapies, like massage and music, are vital to making that period of time special. However, many hospices do not offer these extra services, and that only does a disservice to those who could only benefit from a little extra joy and comfort.
Diana Ramirez – Tri-County Mental Health Center
Funding For Mental Health Services for the Undocumented Population - Tri-County helps individuals within Clay, Ray and Platte counties with behavioral, substance use, and mental health needs but does not have the funding to provide its services to the undocumented immigrant population. The federal government provides the majority of the funds to Tri-County and clients must have a Social Security number to receive services. My role was to find grants that would help the undocumented immigrant population reach mental health services at Tri-County.
Janet Reinke – KU Alzheimer’s Disease Center
Toolkit For a Family Cooperative for Individuals with Dementia - Throughout Kansas, there are a limited number of daycare programs for individuals with dementia. To address this shortage, my Toolkit explains how to set up a care cooperative. A dementia cooperative consists of families that each have a family member with cognitive impairment. The families partner together and the caregivers take turns caring for the family members with dementia. My Toolkit includes relevant legal forms plus information about how to find (and connect with) other such families and important matters to consider.
Annaliese Rosales-Ortiz – USD 500 Kansas City, Kansas Schools Special Education
Menarche And Schools - I noticed the need for clean pants for female students at my school practicum. I wanted to explore the correlation between clothing scarcity for students and their mental health but found there is a need for more research on this. I worked with the school nurse, who typically is the one to provide clean pants to students in addressing the need. Figuring out the correct wording when asking for pants is important so that donations will ensure accessibility to clean pants to all children, no matter their size or gender.
Rachel Sandle – Bert Nash WRAP
Supporting Trans Students by Supporting Teachers - The aim of this project was to determine existing strengths and gaps in the Lawrence Public Schools’ approach to supporting trans students. To do this, the author reviewed existing relevant policies at the state and district level and conducted interviews with relevant policy stakeholders. This project summarizes existing efforts and makes recommendations for changes to support teachers and their trans and gender-nonconforming students.
Paige Sears – North Kansas City Hospital Behavioral Health Navigation
Should My Medical Facility Collect Sexual Orientation and Gender Identity (SOGI) Data? More and more medical organizations are recommending health facilities include Sexual Orientation and Gender Identity (SOGI) questions in their medical intake forms and interviews. The main goal of SOGI data collection is to improve communication between medical staff and LGBT patients with the aim of reducing LGBT health disparities. This presentation also includes sample SOGI intake questions, helpful SOGI collection tips and health related resources for the LGBT community in the Kansas City and Lawrence area.
Jocelyn Segura – KU Health Systems Care Management
Health Literacy: The Hidden Barrier - As part of the integrated healthcare team, I had the opportunity to work with the Radiation Oncology and Gastroenterology teams and patients. While most patients experience some difficulties during treatment, I have seen many patients overwhelmed by their new diagnosis or their loved one’s diagnosis. Patients with low health literacy are more at likely to not understand their diagnosis or condition, mismanage medication, more likely to be hospitalized or need emergency care, are less likely to follow treatment plans, and have higher mortality rates. My project focused on how to work with the interdisciplinary team to reduce these barriers and ensure that all patients are able to access the right information, feel understood, and are empowered enough to ask questions to medial staff in order to make informed decisions for their care or their loved one’s care.
Michelle Smith – University Health Behavioral Health Network
Trauma Informed Care in Behavioral Health Services - My poster highlights the importance of using a trauma informed approach when working with clients in a behavioral health care setting. Trauma informed care (TIC) is a framework that involves understanding, recognizing, and responding to the effects of all traumas. A TIC approach emphasizes physical, psychological, and emotional safety and helps survivors rebuild a sense of control and empowerment. This year at University Health Behavioral Health, I was able to use evidence-based practices to engage clients into services and provide community resources. Integrating a trauma informed approach in a behavioral health care setting has many benefits which can build stronger connections, trust, and provide more effective care for clients.
Calissa States – Camber Children’s Mental Health
Creating Multi-Sensory Environments for Inpatient Facilities - When children experience trauma, they exhibit big emotions that are difficult to manage on their own. Once admitted to a PRTF, children are able to maintain a consistent schedule and learn how to process and manage their trauma in a safe environment. When the facility lacks sensory images or sensory-sensitive design, it becomes difficult for both staff and clients to redirect their dysregulation. Creating a multisensory environment would allow more tranquility and aid employees in teaching healthy coping mechanisms to the patients.
Jodi Steinberg – AdventHeatlh Behavioral Health
Practicing Trauma-Informed Care in the Emergency Department - My practicum at Shawnee Mission Hospital provided the opportunity for me to experience the in-patient unit, the Intensive outpatient unit as well as the Emergency Department (ED). My Capstone project focuses on the use of Trauma Informed Care (TIC) with patients in the ED. I chose to use green and depict a green ribbon on my poster because it is the international symbol for mental health awareness. My poster attempts to explain trauma, trauma-informed and how Advent Health Shawnee Mission utilizes TIC in the Emergency Department.
Emily Stratton – Children’s Mercy
Improving Outpatient Care Outcomes After Mental Health Screening in the Emergency Room - After patients are assessed for mental health concerns in emergency room settings, patients often face many barriers to receiving follow-up outpatient therapy and other mental healthcare. Having a designated hospital social worker conduct a warm hand-off procedure and help patients connect with outpatient resources would engage more clients in follow-up care and reduce the need for return visits to the emergency room, which can be costly and traumatic for patients. Through collaboration within an interdisciplinary and interagency team, emergency room social workers can provide patients with equitable and effective connection to follow-up care.
Addy Turner – USD 500 Kansas City Kansas Schools Special Education
A Safe Space for All Students - All students deserve to be in an environment where they are comfortable, safe and their voices are heard. As a social worker, we should serve as allies and advocates on the behalf of all students. In our schools, teachers and staff should serve as a safe space for students but have not been properly trained to be an appropriate support system for LGBTQ youth. This year alone, has shown the oppression faced by LGBTQ youth especially with the rise of anti-trans legislation. The lives and safety of LGBTQ students are in jeopardy, and someone must have a voice for and with them.
Rachel Wolf – Kids TLC
Language Barriers and PRTF Treatment - According to the National Association of Social Workers (NASW), Social Workers are encouraged to promote diversity, equity, and inclusion to benefit clients despite potential agency or systemic barriers. Language barriers require integrated health professionals to seek bilingual clinicians or interpreters to serve clients. During my practicum at KidsTLC, I was inspired to further my understanding of how the language barrier impacts clients and then consider how social workers can strive towards breaking a language barrier to best serve their clients throughout treatment.
Samantha Wolverton – Four County Mental Health Center
Mobile Crisis Teams in the Assertive Community Treatment Model - While mobile crisis units have been around since the 1960’s, mobile crisis units have become more prevalent with the current emphasis on whole person community-based care. Mobile crisis units meet people where they are to provide assessment, intervention and referral to community services in hopes of avoiding a more restrictive level of care, such as inpatient hospitalization or incarceration. My project was to research and identify the best protocols and practices for a mobile crisis unit that the agency will be launching in the next year.
Rylie Zasypkin-Odom – Children’s Mercy
Trauma Informed Care and Positive PHQ9 Screening in Foster Care Adolescents - This project is looking at depression screening in adolescents who have recently come into foster care and the frequency in which the children are already connected with mental health services. If a child scores high on the depression scale, a proposed additional screening tool will be administered. This will determine if the child is actively engaged with mental health services and if so, gives the child a decision whether or not to meet with a social worker for a further assessment in an attempt to be provide a more trauma informed approach.
View Capstone Projects here
Rebekkah Aarnes Saint Luke’s Health System – Progressive Care (Kansas City)
Brenda Adams Community Health Center-SEK school-based clinic (Pittsburg)
Courtney Alexander Van Go, Inc. (Lawrence)
Gabriella Barnum Swope Health Services (Kansas City)
Tobi Barta Midland Care Connection (Topeka)
Isabelle Bauguess Valeo Behavioral Health (Topeka)
Edan Belihu University of Kansas Health System-Case Management (Kansas City)
Jacob Bigus Interpersonal Psychiatry (Lawrence)
Toni Bond University of Kansas Health System Strawberry Hill (Kansas City)
Kasey Garzillo Bossard Lawrence Public Schools (Lawrence)
Tennyson Clary Family Guidance Center (Saint Joseph)
Mirissa Corbin Truman Medical Center -Hospital Hill (Kansas City)
Olivia Doucas Research Psychiatric Center (Kansas City)
Michele Fields Four County Mental Health Center (Independence)
Chelsea Fluker Children’s Mercy (Kansas City)
Leah Friesen University of Kansas Medical Center Alzheimer’s Disease Center (KC)
Chasity Gaultney DCCCA (Lawrence)
Kristin George Atchison Community Health Clinic (Atchison)
Amanda Graham Community Health Center of Southeast Kansas clinic (Pittsburg)
Brandi Harris Community Health Center of Southeast Kansas (Pittsburg)
Linda Her Southeast Kansas Mental Health Center (Iola)
Jordyn Hudson Children’s Mercy (Kansas City)
Avery Johnson Compass Behavioral Health (Garden City)
Kimberly Johnson Satori Counseling Services (Lawrence)
Kim Keating Pawnee Mental Health Center - Crisis (Manhattan)
Kelsey Klema Blue Valley Schools (Overland Park)
TJ Lakin Four County Mental Health Center (Parsons)
Talita Leikam Children’s Mercy (Kansas City)
Ivette Martinez Children’s Mercy (Kansas City)
Auriana McConnell Truman Medical Center Behavioral Health (Kansas City)
Rachel Parrish KVC Residential Hospital for Children (Kansas City)
Misty Phillips Osawatomie State Hospital (Osawatomie)
Melissa Jones Ramig Goodland Medical Center (Goodland)
Jonathan Ruiz Samuel U. Rodgers Health Center (Kansas City)
Zoey Sallaz Johnson County Mental Health - Addiction & Crisis (Kansas City)
Chelsi Scott Access Family Care (Joplin)
Mikayla Sova Rediscover (Kansas City)
Angela Swetnam Foster/Adopt Connect (Lenexa)
Emma Unsderfer Children’s Mercy/Blue Valley School District (Kansas City)
Bailey Wilson Headquarters Counseling Center (Lawrence)
Ariane Wright University of Kansas Health System-Case Management (Kansas City)
Amber Young University of Kansas Medical Center Primary Care (Kansas City)
View Capstone Projects here
Paola Alor - Olathe Medical Center Oncology
Angela Beims - Salina Family Health Care
Allyson Bence - Community Health Center of Southeast Kansas (Frontenac schools)
Jama Bettis - Lawrence Memorial Hospital Case Management
Anneliese Beye - Tri-County Special Education Interlocal #607 (Independence)
Jasmine Brown - Satori Counseling Services (Lawrence)
Kayla Cosby - Ozark Center New Direction Residential Facility (Joplin)
Alyssa Deem - Community Health Center of Southeast Kansas (Pittsburg schools)
Philip DeGraffenreid - Health Partnership Clinic (Olathe)
Jareth Del Real - Osawatomie State Hospital
Mickey Dick - Visiting Nurses Association (Lawrence)
Alisha Dinges - Kelly Center, Fort Hays State University
Mary Hurchins - Joplin Avalon Hospice
Julianne Jackson - University of Kansas Health Systems Case Management
Tykeisha Kelly - KVC Residential Hospital for Children (Kansas City)
Shelby Lines - Sam Rodgers Health Clinic (Kansas City)
Isabella Meisel - Children's Mercy (Kansas City)
Stefany Ortiz - HealthCore (Wichita)
Viviana Patino - KVC Residential Hospital for Children (Kansas City)
Kristin Quangvan - Saint Luke's Primary Care (Smithville)
Elizabeth Reid - Vibrant Health (Kansas City)
Viridiana Reyes Coria - Crosswinds Counseling and Wellness (Emporia)
Raven Rhoads - St Joseph School District
Jordan Rollins - Ozark Center Community Care Program (Joplin)
Kelsey Savastano - University of Kansas Medical Center Acute Rehab
Katherine Schneider - Mirror- KCK Residential
Desire Seitz - Community Health Center of Southeast Kansas (Pittsburg clinic)
Kelsey Smith - University of Kansas Medical Center Primary Care (Kansas City)
Brenda Alarcon – New Chance (Dodge City)
Treating Substance Use Disorders Together with Trauma - Substance use disorders are treated separately from other emotional or behavioral health disorders. Data shows that individuals who have experienced trauma are at a significantly higher risk of developing a substance use disorder. It also suggests that those who have a substance use disorder are at a significantly higher risk of experiencing repeated traumatic events. To address this cyclical health issue, trauma informed programs such as Seeking Safety, provide an integrated approach to address both issues together.
Claire Albert – Catholic Charities of Southwest Kansas (Dodge City)
Columbia Suicide Severity Rating Scale (C-SSRS): Awareness, Assessment & Prevention - My goal in providing this information to my agency was to advocate for the implementation of the C-SSRS within the programs that are provided by our therapists and staff. Suicide prevention is an important part of every social worker’s assessment. However, you do not have to be clinically trained to be effective at administering the C-SSRS. The questions are simple and use plain language so anyone can ask them. Everyone can be a part of suicide prevention by asking the right questions about suicidal ideation and suicidal behaviors, and then referring on to a trained clinician if necessary.
Jamie Burkhart –Unified School District 347 (Kinsley-Offerle)
Coyotes Rise Up: Resilient-Inspired-Successful-Empowered - The Coyotes Rise Up program at Kinsley Junior Senior High School (KJSHS) is geared towards supporting the student’s social and emotional needs, academic development and success, building resiliency and grit, self-esteem, responsibility, leadership skills, and more. The program consists of small group counseling as well as Leaders in Action. The program was created based on results from the 2019 Kansas Communities that Care survey. The survey showed that students at KJSHS often feel depressed, anxious, and bullied. Students report not feeling empowered within the school such as having a voice or positive relationships. My hope is to create change through supportive relationships.
Christina Dimattia – Unified School District 473 (Chapman)
SBIRT (Screening, Brief Intervention, and Referral to Treatment) in Schools - The influence of substance use on today's youth commands attention. To get a better understanding of its impact, students at a local middle school listened to a brief presentation covering the effects substance use has on the body and decision making after which they completed several SBIRT assessments. Results offered revelations about the prevalence of substance related issues among youth in this rural community. These findings point to schools as an important setting where interventions could be considered essential to prevent and address substance use.
Christian Espinosa – Samuel U. Rodgers Health Center (Kansas City)
Expanding Health Literacy Handouts in a Variety of Languages to Improve Inclusivity and Behavioral Health Psychoeducation -My goal was to promote self-determination to empower clients to participate more directly in their health-care. The simplest most direct way I could contribute was to ensure accessibility of patient education for our recently-arrived immigrant and refugee community. My hope with this project initiative was to review the Integrated Health handouts that were readily available in English, and collaborate with the onsite agency translators to restructure the same information in at least 5 more languages.
Kaitlyn Fernandez – Compass Behavioral Health (Dodge City)
Preadolescent Dialectical Behavior Therapy (DBT) - This poster will explain the core concepts of Dialectical Behavioral Therapy (DBT) and why it would be helpful to teach these skills to individuals prior to adolescence. Most mental health centers that offer DBT offer only adult groups for 18+ or adolescent groups for ages 13-18, I am lucky enough to work at a center who offers both. Through my practicum I have seen a huge need for these skills to be taught prior to the adolescent ages in hopes that if they had the skills taught in DBT they could cope in more healthy ways and avoid self-harm and even suicide.
Lauren Frederick – Children’s Mercy Hospital (Kansas City)
Suicide Prevention in Schools - Children’s Mercy Emergency Room staff assess approximately 200 school-aged youth per month for suicide/homicide/behavioral complaints. The issue of youth suicide in our community is not decreasing. Early intervention and prevention efforts are important for keeping youth safe. This poster is about the findings of suicide prevention strategies utilized within schools in the KC Metro area and by Children’s Mercy. The hope is that Children’s Mercy can use this information to better partner with our community’s school to enhance the prevention of youth suicide.
Laura Hagebusch – Central Kansas Mental Health Center (Salina)
Recognizing and Treating Trauma in Children with an Integrative Approach through Trauma-Informed Schools/Communities – Traumatized youth may experience physical and emotional distress that impacts school performance and impairs learning. Yet trauma affected children are often mislabeled with diagnoses that hinder effective interventions for healing from trauma. There is a need to screen for trauma and develop more trauma-informed treatment plans. This poster features interpersonal aspects of trauma, research highlighting the six key principles of trauma-informed approach and social work roles in assisting their schools/communities in developing trauma-responsive practices.
Alexandria Hall & Brianna Woods – Swope Health (Kansas City)
Emotional Development of Urban Teenage Girls - Over the years research on urban American youth depicts a multitude of ailments that affect their well-being such as higher rates of poverty and discrimination. They also experience more interactions with the criminal justice system while having a lack of healthcare and educational opportunities. The research does not portray how these injustices are affecting the emotional development of African American youth. Therefore, in our capstone project, we aimed to give context to the relationship between systematic barriers and the wellness of Black adolescents. We created a girl's teen group for urban African Americans to gain insight into their emotions. This was accomplished by creating activities and topics of discussions that focused on their unique challenges and emotional development. As the group progressed we observed interesting behaviors from our participants evoked by certain activities.
Devera L. Helwer – City on the Hill (Garden City)
YOLO – You Only Live Once Therapy - Substance use treatment facilities treat alcohol and drug addiction but do not generally address mental health disorders that commonly co-exist with addiction. This poster presents a new therapy tool called YOLO, You Only Live Once, to address co-occurring disorders. It is simple, and it is easy to implement into substance abuse treatment. It may also be beneficial for mental health treatment as well.
Monica Kurz – LMH Health Integrated Crisis Team (Lawrence)
Improving Universal Screening for Suicide Risk in an Emergency Department summarizes a two semester long project conducted in the LMH Health Emergency Department with the Integrated Crisis Team. LMH Health implemented a suicide screening strategy in their triage system in July 2019. To improve the system a fidelity screening tool was created and a random monthly sample of screens was reviewed. Updated training for emergency department nursing and tech staff was created to improve cross disciple understanding of the role of substance use and suicide to eliminate gaps in screening with the Columbia Suicide Severity Rating Scale, a validated screening instrument.
Breonna Lindsey – Rediscover (Kansas City)
The Importance of the Kansas City Assessment and Triage Center - This poster consists of a program overview and a summary of research related to why the Kansas City Assessment and Triage Center (KC-ATC) is needed. Kansas City and surrounding areas are experiencing an increase in individuals suffering from a mental health and/or substance use disorder. This has caused a spike in arrests and hospital visits. KC-ATC was designed to bridge the gap between individuals suffering and access to care.
Consuelo Martinez – Ascension Via Christi Hospital (Manhattan)
Nutrition: An Ally in Reducing Hospital Readmissions - This poster presents how nutrition through proper assessment, inter-professional collaboration, advocacy, and resource education and referral can reduce hospital readmissions. In the hospital setting a social worker will meet with every patient. After the initial assessment, if it is determined that the patient will need further nutritional assessment; the social worker will collaborate with the inter-professional team to ensure the patient receives an advanced screening by the appropriate team member. The poster shows ways a social worker can advocate at micro, mezzo, and macro levels. It also shows a list of Manhattan, Kansas community food resources.
Callie Mauk – Compass Behavioral Health (Garden City)
Trauma-Informed Yoga: Restoring Mental Health through Integration of Mind-Body Interventions - Trauma-Informed Yoga (TIY) programs are specifically designed for engaging survivors of trauma in treatment. These programs demonstrate efficacy in meeting the unique needs of individuals diagnosed with Trauma- and Stressor-Related Disorders in accordance with social work values. This presentation highlights the relationship between mental health and physical health outcomes as well as principles for overall growth defined within TIY programming.
Jennifer McConico – North Kansas City Hospital (North Kansas City)
Bright Beginnings: A Look at Perinatal Mental Health - In a world where mental health is stigmatized, there are many new mothers that are suffering during a time that should be joyous. Research shows that 1 in 7 women who deliver a child will be diagnosed with postpartum depression. Postpartum blues or "baby blues" are experienced by 80% of women who deliver a child. Bright Beginnings is a postpartum support group that was created due to the need for perinatal mental health support. The evidence-based Bright Beginnings Group allows for women to connect with other women who are also experiencing postpartum mood and anxiety disorders (PMAD's).
Amber Meczywor – Cloud County Health Department (Concordia)
Columbia Suicide Severity Rating Scale: Application in Public Health Settings - The Columbia Suicide Severity Rating Scale (CSSR-S) is an evidence-supported tool for suicide assessment. My project involved incorporating the CSSR-S into my own practice and practicum agency routine screenings, educating agency staff on importance of CSSR-S training and triage procedures and motivating staff to complete training to increase awareness, competence, and tools available to handle positive screens going forward. This project reinforced the social worker role in suicide awareness, prevention and intervention.
Lisa Mongold – University of Kansas Health System Saint Francis Campus (Topeka)
Benefits of a Palliative Care Team - Research shows introducing the palliative care team within the first 48 hours can reduce intensive care unit (ICU) readmissions along with the length of stay for patients that are diagnosed with a chronic health condition. As a social work intern in the ICU, I noticed this is a particular concern for patients and their families, and this poster will highlight the importance of the interprofessional team and the national standard for palliative care.
Lindsey Northup – KU Alzheimer’s Disease Center (Kansas City)
The Importance of Social Work Integration for Individuals and Families Navigating Early Stage Dementia - As the number of new dementia diagnoses continues to rise around the world, we cannot expect sufficient emotional support to be provided within the timeframe of an annual neurology or primary care visit. The addition of social workers in dementia care can help to fill these gaps and increase client disease understanding, behavioral management skills, and feelings of competency and preparedness related to continuous disease navigation. Early social work integration provides the unique opportunity for professionals to implement empowering interventions that have the potential to completely transform a family’s experience of dementia.
Madison Noyes – Jayhawk Primary Care (Kansas City)
A Look at How SDoH Has Been Used in Primary Care: Insights from Health Professionals - My practicum, Jawhawk Primary Care, has implemented the use of their own social determinants of health (SDoH) screening tool and data collection. While many health workers can appreciate the connection between social factors and poor health, the actual process of integrating SDoH into routine care can be challenging. This poster summarizes the findings and common themes taken from interviews I held with physicians about their experiences with SDoH. The overall purpose of this project was to examine how SDoH is informing practice and patient outcomes while acknowledging common experiences, challenges, and implications.
Maria Ordonez Vicente – Russell Child Development Center (Garden City)
Program Development in Early Childhood Mental Health - Russell Child Development Center developed a pilot program to meet mental health service needs for children and families. This practicum developed the pilot program and provided in home therapy services to those who experience barriers otherwise. Evidence based programs where combined with one another to teach families in their home environment. Likert scales where used as a measurable way to evaluate success and impact.
Carrie Pfannenstiel – HaysMed (Hays)
Development and Utilization of a Social Determinant of Health Acuity Tool in Community Social Work - With hospital social work moving towards a community and outpatient model of care, acuity tools are essential in monitoring patient progress and tracking staffing needs. Patient success and adherence to medical recommendations is a complex balance interrelated with numerous aspects of their life. Evaluating a patient’s social determinants of health, and assigning an acuity, can aid in understanding and assisting patients overcome barriers to health and wellness. This tracking can also properly reflect a worker’s caseload demands, intensity of patient’s needs, and staffing hours needed to meet this need. While some patients may need short term solution-focused interventions, others will need longer and more comprehensive support. The assessment and assignment of a social acuity will reflect all levels of intervention.
Jennifer A. Robinson – Heartland Community Health Center (Lawrence)
Housing As Healthcare: Social Determinants of Health and Housing Resources and Shortfalls in Lawrence, Kansas - In this poster, I define health and identify the social determinants of health. I then go on to look at the research behind housing as healthcare, identify housing shortfalls in Lawrence and reasoning behind developing a comprehensive housing resource list. Lastly, I discuss implications for social work.
Arnoldo Ruiz Sapien – Vibrant Health (Kansas City)
Behavioral Health Therapy with Hispanic and Latino Populations - This theme was chosen given the disparities I see present within marginalized groups, such as the Hispanic and Latino community, in the United States and rest of the world. There are social, political, economic, and health impacts that oppressed communities, and people of color, face within each of these contexts. By highlighting this information, it gives professionals and a curious audience an insight into the differing bodies and ethnicities harboring within Mental and Behavioral Health spaces.
Stacy Scheetz – Hoxie Clinic (Hoxie)
Mental Health through the Biopsychosocial Model Approach - In today’s society, people are so busy they sometimes forget to stop and think about how important their mental health is when getting their physical health checked during their routine exams. When medical staff and behavioral health staff collaborate and work together, there are better outcomes for the patients they serve. To live happier and healthier lives, we need to educate our communities on how very important it is to take care of ourselves socially, biologically, and psychologically.
Michele Stevens – Compass Behavioral Health (Dodge City)
Reducing Depression thru Yoga in the Elderly - According to the CDC in 2011 and 2012, 49% of long-term nursing facility residents were affected by depression. It was hoped that development of a program in the area would reduce depressive symptoms for residents of nursing facilities with a rapidly aging population. A six week study was conducted using volunteers of Brookdale Senior Living in Dodge City, where chair yoga was introduced to residents by Jyme Cimmamon of Wellness Yoga. Objectives included helping residents reduce depressive symptoms and better adjust to nursing facilities through the use of mindfulness and physical movement. Due to resident safety concerns involving COVID19, the conclusion and presentation was unable to be completed.
Bethann R. Volden – Unified School District 480 (Liberal)
Food 4 Kids- Weekend Food Program for Students Experiencing Chronic Hunger - For my Capstone project, I have started a weekend food program for USD 480 in Liberal, Kansas. The program provides weekend shelf stable food packs provided by the Kansas Food Bank. I decided to start this program because I recognized a need with many students whose families struggle to meet their basic needs at home. Every weekend, a total of 147 food packs are provided to children experiencing chronic hunger.
Rebecca Winterburg – University of Kansas Health System Family Medicine (Kansas City)
Initiation of Universal Substance Use Screening in Primary Care - It is recommended that all adults age 18 years or older be screened for substance use. The Family Medicine – Interprofessional Teaching Clinic at University of Kansas Health System will implement and study the initiation of universal screening substance use. Through screening efforts, the clinic will examine what components of the screening process can be adjusted to improve patient experience and the referral process.
Abigail Baldwin – AdventHealth (Shawnee Mission)
Involuntary Behavioral Health Patients in AdventHealth’s Emergency Department - AdventHealth’s staff has noticed increasingly high numbers of involuntary behavioral health patients in the emergency department(ED). Due to this, it was clear that creating a data tracking system would be helpful. Analysis of this data provided valuable information related to this population of patients that will be presented to management and the State of Kansas. This information includes but is not limited to demographics of the population, average time patients spent in the ED, associated hospital costs, and recognition of the distance patients traveled to reach the ED. This data also highlighted the importance of increased assistance and employment of behavioral health clinicians which would benefit the department during peak volumes.
Marcelo Benalcazar & Andrea Davis – BullDoc Clinic at Wyandotte High School (Kansas City)
The Importance of Regular Trauma Informed Trainings in High School Setting - With the rise of school shootings, racism, parents removed by immigrations enforcement and other significant stressors, it is of utmost importance to make sure that trauma informed care is put into the forefront of curriculum for teachers and staff. Our poster will argue the benefits of ensuring that the administration and staff of high schools are properly trained in helping adolescent aged children get through the variety of traumas that can occur on a day to day basis. We have been witness to a number of insensitivities from teachers when dealing with those from marginalized populations. We believe this to be the best route to take. The hope is that with the poster, we can properly make our thoughts and concerns known in a way that will teach and positively benefit those around us.
Elizabeth Burris – AdventHealth Shawnee Mission Primary Care (Shawnee Mission)
Implementing Patient-Centered Practices in Primary Care Clinics - Research has consistently shown positive outcomes for patients when both primary and behavioral health care interventions are utilized in treatment. Having health care providers that use principles of patient-centered care such as care coordination, accessibility/continuity of services and valuing patient preferences are vital to service delivery. This poster will examine research on the efficacy of patient-centered practices, and how social workers at AdventHealth Shawnee Mission Primary Care have implemented these practical interventions.
Monica Cabrera – Vibrant Health (Kansas City)
Trauma Informed Design for Integrated Healthcare Settings - This poster will define the concept of “trauma informed design” and explain the need for it in integrated healthcare settings. Supporting research along with specific examples of how it can be implemented will be offered including examples from my field practicum at Vibrant Health.
Cathy Carroll – Community Health Center of Southeast Kansas (Pittsburg)
Medication Assisted Treatment - The United States is currently experiencing an opioid epidemic. In part, this epidemic is a result of medical providers attempting to minimize their patients’ physical pain while pharmaceutical companies engaged in marketing and educational outreach to assure both physicians and consumers alike that the opioid medications were non-addictive. Community Health Center of South East Kansas (CHC/SEK), a Federally Qualified Health Center (FQHC), currently provides Medication Assisted Treatment (MAT) at the Pittsburg location; however, due to the rural location and lack of transportation there are many individuals unable to access this resource. With the addition of the Fort Scott clinics CHC/SEK has an opportunity to now, or in the future, help individuals find recovery who would otherwise be missed.
Lucy Cummings – VA Medical Center (Leavenworth)
Strengthening Service Delivery by Developing Implicit Bias Awareness - Our brains routinely, and often unconsciously, notice patterns and make generalizations. For example, at a young age we learn fire=dangerous. Associations are not only crucial for survival, but also help make sense of the world. However, they also create barriers to equity and opportunity. This poster overviews a workshop on implicit bias that we facilitated for social workers at the Leavenworth VA. Learning objectives include: increase education and awareness about implicit bias; enhance understanding of how implicit bias impacts social work practice and integrated healthcare service delivery; and identify strategies for reducing the negative impact of unconscious bias. Co-author: Annie Lemmon
Megan Davies – Konza Prairie Community Health Center (Junction City)
Konza Cares: Breaking Down Barriers to Receiving Care - As a Federally Qualified Health Clinic, Konza Prairie Community Health & Dental provides integrated care in a medically underserved community. While this promotes healthcare access to the greater population, barriers to receiving care are still prevalent. In hopes of reducing these barriers, Konza Cares was established as a financial assistance program to help address clients’ needs such as transportation, medication coverage, and copay coverage.
Brittany Dwyer – St. Luke’s Health System- NICU (Kansas City)
Striving for a Better Future: Bringing Awareness to the Health Disparities that Exist for Black Mothers and Infants - Research shows that the risk of pregnancy related deaths for Black women is 3-4 times higher than those of White women. Additionally, the infant mortality rate for black infants is 11.1 deaths per 1,000 live births, while for white infants it is 5.2 deaths per 1,000 live births. These statistics highlight the incredible disparities that exist in health care settings for Black women and infants however, it is also equally important to look beyond the statistics to create a better and safer future for all women and infants.
Laura Edwards – Complete Circle Counseling and Coaching (Wichita)
Mental Health Therapy Groups for Children - My poster will consist of the program overview, information regarding my practicum, summary of the research related to this, and anything social workers need to know about group therapy for children. This topic is one that I believe should be utilized in mental health facilities, but one that I have not seen a lot of outside of psychiatric hospitals. I feel that it is important to provide group therapy experiences to children to improve social skills, modify behaviors, and learn to work well with others.
Carmen Engelke – First Care Clinic (Hays)
Stress Less: Identifying and Managing Everyday Stress and Anxiety - The American Institute calls stress and anxiety, "American's leading health problem", representing the most common mental illness in the United States and affects 40 million adults in the country every year. Consistent high levels of stress or anxiety can cause people to develop conditions such as hypertension, stroke, diabetes, chronic pain, and heart attacks. Identifying the causes of daily stress and anxiety is the first step to leading an overall healthier life, followed by developing positive coping skills to manage stress and anxiety to reduce the negative effects on our health.
Vanessa Gaytan & Juan Vicente-Ramos – Genesis Family Health (Garden City)
Telehealth Utilized to Improve Behavioral Health Services at a Western Kansas FQHC -Telehealth has been utilized for over 40 years in the medical profession, however, primary care in Southwest Kansas has yet to maximize the service. With rural Kansas having limited specialists and services, recently initiated telehealth services at Genesis Family Health has been used to improve behavioral health access to patients. Since the utilization of telehealth at Genesis Family Health, there is an increase in psychiatric clientele and will be expanding to provide therapeutic services in 3 other Southwest Kansas locations. Our project is focused around usage and expansion of telehealth services in order to provide more accessible healthcare needs in all other Genesis Family Health locations.
Madelin Greer – St. Luke’s Health System- OB/GYN (Kansas City)
Becoming a Mom: Group Prenatal Care for First Time Moms and the Importance of Education and Self Care - Becoming a Mom is a prenatal group for first time mothers that is based on education and group support structured after the Centering Pregnancy Program. These programs reduce emergency room visits in the third trimester as well as increase the new moms’ readiness for labor and delivery. While this group mentions postpartum depression, it lacks a focus on self-care and coping mechanisms that these moms can implement in their day to day lives. This project focused on educating new moms on their pregnancy as well as teaching self-care practices to be used postpartum to help reduce stress and take time to take care of themselves.
Nancy Guzman – Compass Behavioral Health (Garden City)
Engagement Opportunities - My work at Compass Behavioral Health includes working with boys and girls psychosocial groups and doing individual therapy at the local jail and detention center. In my work, I have found that there are many resources that people do not know about in Garden City. My poster presents local resources in the areas of self-care, emergency financial aid, emergency housing, family support services, clothing, mental health support and children’s services.
Meagan Howard – Research Psychiatric Center (Kansas City)
The Impact of Voter Engagement on Health Outcomes - El Centro, Inc. initiated the Integrated Voter Engagement (IVE) project through the Advocacy and Civic Engagement department as a strategy to actively engage Kansas residents to become advocates for change through common issues campaigns. Community action events will aid in measuring voter registration, voter turnout, voter literacy, and leadership building. The desired goal is to achieve policy reform with a specific focus on health outcomes and to implement a bill/policy that is catered to the communities' health needs.
Bethany Knipp – Cottonwood Springs (Olathe)
Engaging Support Systems Following Mental Health Diagnosis - How can family, friends and other support networks best support a loved one following a mental health diagnosis? There are steps that both people with mental health diagnoses and their support networks can take to help in times of crisis and times of mental health maintenance. Proper support can provide better outcomes for people with mental health diagnoses, so what do we do?
Kendra Konrady - Research Psychiatric Center (Kansas City)
Introducing Motivational Interviewing to Nursing Students - The purpose of this capstone project is to provide an overview of Motivational Interviewing to nursing students. Through didactic instruction and interactive demonstrations, the students were trained to provide brief interventions for patients across multiple healthcare settings. Students were taught to utilize the importance and confidence rulers that help patients resolve ambivalence and assist providers with understanding the patient’s readiness to change.
Karla Martinez – Great Bend Schools (Great Bend)
Integrating Mental Health in School Curriculum - Amid sharply rising rates of teen suicide and adolescent mental illness, some states have enacted laws that for the first time require public schools to include mental health education in their basic curriculum. Great Bend High School has joined a small group of schools integrating social emotional curriculum into school hours in hopes of helping address their students’ mental health. By educating children of all ages about mental health, the hope is that they will learn how to recognize early symptoms in themselves and their friends and seek help before a crisis develops.
Traci Martinez – Garden City Schools (Garden City)
Columbia Suicide Severity Rating Scale (C-SSRS) - While suicide is the 2nd leading cause of death amongst the ages of 10-24, interventions such as the Columbia-Suicide Severity Rating Scale have been developed to decrease that number (NIMH, 2016). Mental health has been on a rise and affects much of our youth in today’s society. Garden City High School has started to implement Trauma Informed Care into their district wide training. Students, faculty, and administration would benefit from becoming educated and aware of evidence-based practices like the C-SSRS to prevent suicide attempts and completions. The implementation and utilization of the C-SSRS can act as a beneficial tool before a crisis occurs.
Alexandra C. Mellor – Lawrence Memorial Hospital (Lawrence)
Do I Really Need a PCP?: The Vital Importance of Having a Primary Care Provider - In my work at Lawrence Memorial Hospital, I frequently encounter individuals who do not have a PCP due to a variety of barriers that limit access. As an intern under a PCP at Heartland Community Health Center last year, I have been able to learn about the inner workings of our local FQHC; thus, this year a main project of mine has been to see any patients that enter the General Medical Unit without a listed PCP and provide education, resources, and assistance setting up appointments to help them establish care. Having a PCP can help patients manage their chronic health needs and reduce how often they readmit to the hospital; in turn, this helps patients more readily meet their health goals, maintain progress made medically, and develop more effective regimens for management.
Shanna Prescott – Smoky Hills Foundation (Hays)
Incorporating Mental Health Professionals in Outpatient Substance Abuse Treatment Facilities - Clients with co-occurring disorders would greatly benefit from the incorporation of mental health professionals in substance abuse treatment facilities. These substance abuse treatment programs could provide a safe forum for discussion about medication, mental health, and substance abuse issues in an understanding, supportive environment wherein coping skills can be shared.
Kristen Rawls – The Children’s Shelter (Lawrence)
Meeting the Changing Needs of the Community: The Path from Congregate Care to Qualified Residential Treatment Program - The children in our residential group homes have very unique challenges. Most of the youth in our facility come to us after being removed from their home due to abuse and neglect via referral from the state child welfare contractors. Consequently, many of our youth are in crisis upon acceptance into the group home. Although our case managers scramble to get mental health needs met, at best, youth are without treatment for a few weeks. This is a systemic failure as the average length of stay in our facility is only 29 days. To better meet the needs of this population, an organizational change towards more trauma informed care is needed. This poster presentation highlights the research that led to the decision and the steps that have been taken to move in that direction.
Michal Rogers – University of Kansas Medical Center Family Medicine (Kansas City)
Self-Care for Health Care Students -Statistically, health care providers are at an increased risk for depression, anxiety, and suicidal ideation. Students in the health care field report high levels of stress and burnout, which can lead to mental health problems, compassion fatigue, and decreased quality of care. At the Interdisciplinary Training Clinic (IPTC) at University of Kansas Physicians (UKP) department of Family Medicine, students from a variety of disciplines collaborate to treat patients. Using a psycho-education, lunch-and-learn workshops, and a resource library, this presentation highlights the benefits of addressing self-care with health care students of the IPTC.
Grecia Rubio – St. Catherine’s Hospital (Garden City)
Implementation of C-SSRS Suicide Assessments in Rural Areas - Suicide prevention is a topic of national importance and identification of at risk individuals is the first necessary step toward prevention. Screening for suicidal ideation and behavior should be integrated across public health settings and made as routine. It is of extreme importance to make a significant potential change in our country's rural areas where research demonstrates an increase in suicide rates.
Jacob Schooler – Valeo Behavioral Health Care (Topeka)
Ethical Use of Adverse Childhood Experience Assessments in Primary Care Facilities - Efforts to create programs designed to prevent health concerns and build resiliency in children who experience adverse events have been successful. Currently most adult focused programming is centered on preventative work for families. As more primary care facilities are becoming invested in an integrated model, there is a greater desire to use existing research in behavioral health developments. To ensure the ethical use of ACE assessments, this poster will examine the limitations and requirements of using such technologies with adults in a primary care setting.
Shari Taylor – St. Luke’s East Hospital (Lee’s Summit)
What is Palliative Care? - What is palliative care and how can it benefit patients in healthcare? This poster will be an education piece to give the overview of what palliative care is and when it would be most appropriate for patients to improve life. There are a limited number of agencies within Kansas City that offer this level of care.
Samantha Trujillo – KU Pediatrics (Kansas City)
Postpartum Depression: Creating a Mom's Support Group - My poster highlights a once a week support group for women who are pregnant; or, have recently given birth and are experiencing anxiety, depression or unwanted thoughts or behaviors. The purpose of this support group is to help educate, empower, and provide hope during pregnancy and after the birth of the baby.
Jessica Albin – Kelly Center (Hays)
CarePortal: Creating Avenues for Local Churches to Support Children & Families in Crisis - The turnover rate for foster families is extremely high. CarePortal is a Christian agency that seeks to build connections between local churches with children and families in crisis through supporting current foster families, increasing awareness of fostering and meeting material needs. This poster will describe the work of CarePortal and ways for social workers to utilize this beneficial platform.
Fernando Alvarez & Becky Clark – Genesis Family Health (Garden City)
The Power of Connection: Increasing Engagement with Children and Adolescents in Therapeutic Settings The basic foundational component for the therapeutic process is the ability to create and maintain a positive, proactive connection with our clients. The relationship we create with the clients is the single most important factor in a successful outcome. Creating and maintaining a connection when working with children and adolescents can be a complex challenge. Our project is designed to provide the clinician with basic skills and tools to create that connection for maximum therapeutic benefit.
Robyn Ashauer – Heart of Kansas Family Healthcare (Great Bend)
Use of Interpreters in the Therapeutic Process As America becomes more diverse the population of people that do not speak English grows. As most mental health practitioners are not multilingual, this leaves clinicians having to find some way to work with these populations. For most practitioners, that will be through the use of interpreters. This poster will examine current literature to determine the efficacy of meeting client needs in this way and identify best practices in this area of mental health service provision.
Jared Auten – Bert Nash Health Connections (Lawrence)
Peer Support Network: A Collaborative and Peer-Led Approach to Addressing Mental Health Needs on Campus The Peer Support Network (PSN) is a KU student organization created by students with the support of professionals and agencies in the community. This poster will present the rationale and timeline in the creation of the PSN, along with a brief review of the literature to support the use of peer based supports in higher education. It will highlight successes of the collaborative approach and limitations/challenges.
Jacey Bishop – Johnson County Mental Health Center (Olathe)
Domestic Violence Survivors and Mental Health: What Happens When They Intersect? - Survivors of domestic violence often have long-lasting mental health issues as a result of various forms of abuse (physical, psychological, etc.). Mental health and domestic violence are almost always intertwined, whether through the abuser, victim, or children who witness the abuse, yet many services for survivors are not equipped to handle the symptoms that come with severe and persistent mental illness.
Vivien Brite – Stormont Vail (Topeka)
A 2017 Snapshot of HealthAccess Recipients - The Shawnee County Medical Society (SCMS) HealthAccess program helps connect low-income, uninsured residents with donated medical care, hospital services, and medication assistance to complement the work of local community agencies. To contribute to existing literature regarding social determinants of health, researchers examined the characteristics of hospital/ clinic patients referred to HealthAccess for 2017. Co-authored with Sabrina Robinson, BSW & Karla Hedquist, Executive Director of Health Access
Shelby Covey – Kids TLC (Olathe)
What is Continuity of Care? Continuity of Care is defined as longitudinal or provider continuity during the course of treatment. It is flexible, meets evolving needs of the client, and provides consistent therapeutic services after discharge. Wrap around services may include: case management, medication management, in-patient services, outpatient services and additional therapeutic services. Providing these services upon discharge lowers a client’s risk of regression as well as possible lapse of care.
Alex Creech – Heartland Community Health Center (Lawrence)
Smoking Cessation & Integrated Healthcare Research shows that individuals who are in recovery of a substance and also quit smoking cigarettes are twice as likely to not relapse. Smoking Cessation is uniquely provided to everyone who is a patient at Heartland Community Health Center, as well as through First Step at Lakeview, a residential program through DCCA. Smoking Cessation and integrated care increase the likelihood of an individual to quit and stay sober from smoking cigarettes.
Lyndsey Crisenbery – Hays West Central Kansas Special Education Cooperative (Hays)
Foster Care to Prison Pipeline - Nationally, one-quarter of foster youth and two-thirds of “crossover youth” (foster children who enter the juvenile delinquency system) have a jail stay in early adulthood. These youth are at greater risk for involvement in the justice system due to experiences with abuse, neglect, and home removal along with poverty, community instability, parental incarceration and parental substance abuse and mental health issues. This presentation will start a conversation about how we can help support our foster youth, and improve services in order to reduce this trend.
Chrissie Diehl – Johnson County Mental Health Center (Olathe)
Efficacy of Equine Assisted Learning (EAL) & Equine Assisted Psychotherapy (EAP) - Equine Assisted Learning (EAL) and Equine Assisted psychotherapy (EAP) is an alternative therapeutic approach using horses to help reflect clients non-verbal incongruencies, enhance personal growth and development and address mental health concerns. The effectiveness of merging this experiential holistic approach with solution-focused-therapy (SFT) and other evidenced-based treatment modalities such as ACT, EMDR, and CBT continues to be heavily researched in universities around the world.
Nicole Franklin – Marillac (Overland Park)
Life Skills for Millennials in Alternative Education - Do you know how to sew on a missing button, file taxes, or register a vehicle with the DMV? These are tasks that millennials in alternative education may not have the opportunity to learn before graduating high school. At S.O.A.R. alternative high school, we developed a psycho-educational “Adulting 101: Basic How-To’s for Life” group for juniors and seniors. “Adulting” groups are a growing trend across the nation offering a supportive setting for learning new life skills.
Heidi Goerzen - Prairie View (Newton)
Connectedness as Prevention for Adolescent Suicide Adolescent suicide is a public health problem in the United States. Because of this, prevention strategies are needed. Research suggests that connectedness and a sense of belonging for adolescents can help prevent suicide. As social workers can help build connections in many avenues with adolescents, we can be at the forefront of suicide prevention through connectedness-based interventions and strategies.
Mayra Gonzales – Compass Behavioral Health (Dodge City)
Yoga Calm: Integrating Mindfulness in the Classroom - My project will emphasize the importance of whole-person education in the classroom. I will focus on Yoga Calm and its benefits that cater to students’ physical, mental, and emotional aspects. I will present a brief description of the program and how it supports students in developing various skills and techniques. I will highlight some of the research that endorses Yoga Calm, which promotes physical movement, mindfulness, and emotions in the classrooms.
Alyson Gordon – Larned State Hospital (Larned)
The Effects of Decreased Funds for Mental Health on Admissions to Larned State Hospital State Security Program For many years, mental health programs have felt the sting of funding cuts. This poster will explore if admissions for evaluation orders have increased as funding has decreased. Additionally, it will be studied if 18-25 year-olds are admitted at similar rates as the rest of the population.
Matthew Jepsen – Pawnee Mental Health Center (Manhattan)
Through the Eyes of Body Dysmorphic Disorder - Body Dysmorphic Disorder (BDD) is a mental disorder in which a person is preoccupied with an imagined physical defect or a minor defect that others often cannot see. As a result, people with this disorder see themselves as ugly, even disfigured, and often avoid social exposure. The most common treatment used to help individuals with BDD is Cognitive Behavioral Therapy (CBT). This poster presents additional strategies that can be used to minimize the effects of BDD.
Dorian Jester– Johnson County Mental Health Center (Overland Park)
A Fallen Voice: Family Narratives of those under Correctional Control - Narrative Criminology is an ideology, which posits that stories are more than a means of communication -they help us mold our identities, make sense of the world, and assemble others to action. This research explores the personal narratives of offenders under community correctional control to explore how stories are used to explain their unique experiences.
Alison Kuhn– PACES (Kansas City)
Resiliency: Why Does It Matter in Social Work Practice? - Resiliency plays a role in our ability to adaptively respond to traumatic events, tragedy, and various life stressors. Social workers can help build resiliency by utilizing a strengths-based perspective and shifting the clinical approach from “what is wrong with you” to “what has happened to you.” Utilizing knowledge of protective factors that foster resiliency, social workers can approach individuals and families in a more holistic manner that promotes sustainable solutions and overall better health outcomes.
Ja’Lynn Montgomery– Raymore Peculiar High School (Kansas City)
Utilizing Yoga with Youth in Educational Settings - Utilizing yoga breathing and meditation techniques during therapeutic groups and individual sessions helps children and adolescence in many ways. This poster discusses the school social work team at Raymore-Peculiar high school utilizing yoga techniques through stress, anger management, and Attention-Deficit Hyper Activity Disorder psycho-educational groups. It also discusses the research of this evidence based practice and its successes with youth in educational settings.
Kaylee Murphy – Children’s Mercy (Kansas City)
Screening for Depression in a Pediatric Care Center - Children’s Mercy Hospital has implemented an emotional health initiative to help identify depression among patients 12 years old or older using Patient Health Questionnaires including the PHQ-2 and PHQ-9. This poster will discuss validity of the questionnaire tools, description of implementation within the Pediatric Care Center Broadway Clinic, the social work process and follow up, and Children’s Mercy’s efforts to implement a more universal screening tool including the CSSR.
Derion Rusley – BullDoc Clinic (Kansas City)
Conflicts of Maternity Leave - Research shows that individuals who are in recovery of a substance and also quit smoking cigarettes are twice as likely to not relapse. Smoking Cessation is uniquely provided to everyone who is a patient at Heartland Community Health Center, as well as through First Step at Lakeview, a residential program through DCCA. Smoking Cessation and integrated care increase the likelihood of an individual to quit and stay sober from smoking cigarettes.
Kristyna Smith – Van Go (Lawrence)
Van Go Works! - Van Go is a local, non-profit with a unique vision for the delivery of social services skillfully tailored to the community of Lawrence. Their mission is “To improve the lives of high-needs youth using art as the vehicle for self-expression, self-confidence, and hope for the future.” They serve both youth and transition-aged youth, ages 14-24 through employment training by hiring individuals to make art, learn valuable Go Healthy Life Skills, and receive supplemental social work services, funded by the federal Workforce Innovation Opportunity Act grant, community contributions, and the sales of their art.
Baillie Woydziak – Children’s Mercy (Kansas City)
Mental Health 911- Providing Trauma Informed Care in Pediatric Emergency Departments - Pediatric Emergency Departments are experiencing an increase in the number of emergency psychiatric patients each year. This poster discusses the need for an increase in mental health training and collaboration across pediatric care systems. The goal is to inform and empower individuals working with adolescents on how to respond therapeutically when a child is experiencing a crisis. In turn, patient care will be more effective and improve outcomes.
Connor Wyckoff – Johnson County Mental Health Center (Olathe)
DBT with Young Adults - Dialectical Behavior Therapy is a relatively new type of therapy, but it has been shown to work with a number of different populations. DBT teaches skills that everyone can benefit from, especially young adults who are facing a transition stage of life. A commitment to DBT requires weekly individual and group sessions. DBT is broken down into four main areas: Mindfulness, Emotion Regulation, Distress Tolerance,
Katie Barger – Bert Nash WRAP (Lawrence)
The Power of Positive Connection - When working with children, teens, adolescents, or even adults, if there is not a rapport or positive relationship, the likelihood of success and efficacy are slim to none. As human beings, we strive to love and be loved and it is relationship and positive connections that allow us to learn, grow, and develop the skills needed to be successful. The work of Bruce Perry and the idea where he states "Relationships are the agents of change and the most powerful therapy is human love” is a key factor to remember as social workers and as any professional working with kids and with people in general. In a school setting, it can seem that some of the work we do may not impact a whole lot but when you look at how powerful relationships are, those positive connection leave a lasting impact on development and success.
Drew Belanger – KU Counseling and Psychological Services (CAPS) (Lawrence)
The Effects of Childhood Trauma on College Students Relationships - Childhood trauma follows children through adulthood and manifests itself in a variety of ways when these young adults seek relationships, whether they be friendships or intimate partnerships. The goal of this poster is to explore the ways in which symptoms of trauma manifest itself in relationships. Briefly, this poster will explore brief interventions for trauma survivors, providing a hopeful outlook for these individuals.
Amanda Brunk-Grady – Heartland Health Clinic (Lawrence)
Integrated Primary Care - When general medical providers collaborate with mental health specialty providers, the result is integrated care. Instead of patients needing to seek care in multiple locations with providers who may never communicate with each other, integrated care allows for the patient to have their primary care and mental health needs addressed collaboratively, often under one roof. An integrated primary care model can increase patient access and engagement.
Haley M. Doubrava – Stormont Vail West (Topeka)
Cluster Suicides in High Schools - First, of all my presentation will clearly state the criteria of cluster suicides. Then, I would like to identify any risk factors of students or the environment related to cluster suicides. Next, I would like to discuss post-suicide interventions for schools to take in order to prevent future suicides. Lastly, I would like to touch on some suicide prevention strategies that schools can implement or have implemented.
Madeline Ford – Children’s Mercy (Kansas City)
Implementation of the Patient Health Questionnaires in a Pediatric Primary Care Clinic - Children’s Mercy Hospital has implemented Patient Health Questionnaires (PHQ-2 and PHQ-9), which are brief depression and suicidal tendency screening tools, at multiple locations in Kansas and Missouri. The poster will cover a brief overview explaining the validity of the questionnaires, along with visual aids of the implementation process at CMH West Clinic, the screening tool itself, and the social work follow up process. Finally, a short case example will be given as a take home message.
Ashley Granville – Family Service & Guidance Center (Topeka)
Collaboration and Continuity across the Children’s Mental Health Systems - The mental health system is complex and can be difficult to navigate not only for our clients, but also for the professionals working within the system. This presentation will discuss the importance of collaboration from the micro to macro levels. The goal is to identify successes and challenges in the current system, and highlight how new research on trauma and integrated care are changing the way we practice. When social workers are able to efficiently and effectively collaborate children and their families are more likely to gain the resources and skills necessary to succeed.
Kori Godinez - Kansas City, Kansas Schools & Jennifer Holder – Olathe SOARS
Working with Transgender Adolescents in the School Setting - Our topic is on supporting Transgender youth in the school setting. It will surround the risk and protective factors Transgender youth face, how school social workers can support their needs, and the need for development of legislation surrounding protection of Transgender youth in a school setting.
Chelsea Harrington – Wyndot Center (Kansas City)
Early Intervention for Young Adults in their First Episode of Psychosis - My poster will highlight information from the RA1SE (Recovery After Initial Schizophrenic Episode) research which led to the development of the NAVIGATE program. I will briefly touch on how the NAVIGATE program functions (the different team members roles) and provide more specific information on Individual Resiliency Training. I will also include some of the challenges we (Wyandot Center) have come across in implementing this program as well as some modifications we have made.
Catelyn Holmes – Maddie Rhodes Center (Kansas City)
Trauma Informed Care in Schools - The purpose of this poster is to show how Mattie Rhodes Center has developed a way to incorporate Trauma Informed Care into the school system. By sharing knowledge from one discipline to another, students can receive care that encourages their academic success and personal resiliency. The monthly Trauma Informed Care Newsletter is one of the ways that Mattie Rhodes Center is creating trauma awareness in the school and is positively influencing students.
Cari Hommertzheim & DaKie Washington – The Villages, Inc. (Topeka)
The EASY PEASY List - The EASY PEASY list has been designed for working with youth ages 10-18. This is a positive reinforcement initiative program designed at improving behaviors among youth in a YRCII placement.
Marissa Kile – Marillac (Kansas City)
Social Media's Effect on Adolescent Mental Health - The use of social media is a new norm in adolescent daily life. Although negative effects of social media on mental health are most often reported (i.e. cyber-bullying, sexting, depression), there are also benefits. Researchers have found social media can create social capital, improve self-esteem and provide increased access to mental health resources. It is important for social workers to be aware of various social media sites to encourage healthy and safe use, especially among adolescents
Laena Loucks – Johnson County Mental Health Center (Olathe)
Mental Health Literacy in Schools: A Needed Partnership -The National Alliance on Mental Illness reports that approximately one in 5 adolescents aged 13-18 have or will have a serious mental illness (NAMI). Mental health in schools is not given the same importance and focus as physical health. Implementing mental health literacy curriculum in the classroom beginning in kindergarten, may serve to reduce stigma, bullying and increase early intervention for students struggling with mental health issues.
Hannah Lujano – The Shelter, Inc. (Lawrence)
Successful Positive Behavior Support Practices for the RevolvingDoor of Juvenile Out of Home Placement - I have chosen to present on the implementation of effective positive behavior supports in youth residential centers. While most of the group homes I have experienced are functioning under the assumption that they are already using positive behavior supports, their systems of enforcing structure has fallen into punitive measures of punishment and disregarding the framework of PBS. I will meet with a representative of the Kansas Institute for Positive Behavior Supports to collaborate with them in order to guide the local groups homes back to a system of positive behavior supports that provides structure for staff and residents alike.
Alli McGuinn – Priority Care Pediatrics (Kansas City)
Transitions in Pediatric Primary Care - Navigating the health care system is challenging for most people, but especially for adolescents and young adults who often have limited experience in managing their own health care. Transition age youth are a vulnerable population in general and individuals with special health care needs can struggle with transitioning from pediatric medical care to adult primary care. This presentation is aimed at laying out a transition process to be used in pediatric primary care settings, with focus on individuals with special health care needs. Aspects of this process that will be addressed include adult skills the patient will need to develop throughout adolescents, how medical staff and family members can provide support, and the resources available to assist with transition.
Nicole Neves – YouthThrive (Overland Park)
Importance of Relation Permanence in Foster Youth - This poster will serve to outline the need for relation permanence in foster youth. With only 3% of foster youth obtaining a college degree and only 58% graduating high school the need to have positive transitional support is high (Youthrive, 2015). Statistics will show that having a stable relationship that lasts longer than a year is more likely to withstand the long term; thus creating lasting positive support as youth transition into adulthood. The cost to both the state and the youth can be decrease through relational permanence.
Nicole Olivier – BullDoc (Kansas City)
Becoming Trauma Informed and its Effects on Student’s Behavioral Health - Many of the students we serve at BullDoc have generational and historic trauma that reflect systemic oppression. Thus, it is important for social workers in the school system to be able to recognize trauma and acknowledge its impact on brain development and behavior. As social workers, one of our roles is to educate the school personnel on its effects on the development of the survival brain versus the learning brain. We must also advocate and explore strategies for supporting and connecting with challenging students who may have a history of trauma. From this perspective, we must examine “triggers” and “de-escalation” strategies for intervening in the traumatic response and supporting trauma impacted youth. We must also shift from “What happened to you?” and move towards “How can we shift the school environment and classroom practices to respond more effectively to needs of these students?”
Natalie R Reeves – Kansas City, KS Schools
How Nutrition Can Impact Aggressive Behavior - Aggressive behavior causes many problems in society and has wide impacts. Recent research has found that aggressive behavior can be reduced substantially by adding Omega 3 fatty acids to individuals’ diets. These findings prove further, how nutrition impacts behavior and how disadvantaged populations who do not have access to adequate nutrition are put further at risk. It also offers solution to an issue that the United States spends billions of dollars on each year.
Giselle Scott – Van Go (Lawrence)
Why Self-Care Can Be So Difficult, & Why Social Workers Should Be Striving To Normalize It - Ideas and reflections about how American culture discourages self-care. This poster aims to stimulate conversation about guilt as an intruder of healthy self-care, and the audience is encouraged to interact directly with the poster by writing in responses to the prompt "Share a Self-Care Moment that Made You Feel Guilty" in the designated writing space. Recommendations are made regarding why the overall health of the social work field depends on the field-wide cultivation of a healthy self-care culture.
Stevie St.Clair – Bert Nash Health Connections (Lawrence)
Wilderness Therapy Effectiveness - Wilderness therapy is an experiential holistic approach, incorporating mental, physical, and emotional aspects of a person. As a newly accredited therapy treatment, both positive and negative implications have developed. Ethical concerns surrounding wilderness therapy include the safety, efficacy, and continuum of care.
Kelsey Wendland – PACES (Kansas City)
My Client has ACEs—Now What? Pairing Resiliency Interventions with ACEs Assessment - Significant research has illuminated the profound negative effects that adverse childhood experiences (ACEs) can have on an individual. While it is helpful to assess for ACEs with awareness of the potential damage they can do, social workers and clients alike may feel helpless orunsure of how to move forwardonce they have assessed for ACEs. So how can clinical social workers respond effectively to ACEs assessment? This is where resiliency factors come into play. This presentation examines one intervention designed to increase resiliency factors with clients who are at high risk for or already have multiple ACEs.
Bria & Briana Williams – Samuel U. Rodgers Health Center (Kansas City)
The Future of Integrated Care - Since the early 1960s, research has indicted an estimate of 70% of primary care visits stem from psychosocial issues, yet in a traditional primary care model, practices do not include behavioral health providers. This poster will discuss the integration of behavioral health in primary care, the role of a Behavioral Health Consultant, and the implications for social work practice. Presenters will highlight Missouri’s Primary Care Health Home Initiative within the context of a Federally Qualified Health Center.
Dairi Amaya - Maddie Rhodes Center (Kansas City)
Stephanie Andrasek - St. Francis Community Services (Great Bend)
Joanna Bustamante - Compass Behavioral Health (Garden City)
Lindsay Dunlap - Van Go, Inc. (Lawrence)
Rebecca Esparza - Maddie Rhodes Center (Kansas City)
Donna Finley - Goodland Family Health Center (Goodland)
Eric Fitzmorris - Lawrence High School/CTRAN (Lawrence)
Nadina Goddard - Bert Nash WRAP (Lawrence)
Ginny Helgeson - Wyandot Center Health Homes (Kansas City)
Johana Hernandez - Garden City Schools (Garden City)
Diane Hughes - Heartland Community Health Center (Lawrence)
Ada Jarrar - The Family Conservancy (Kansas City)
Eric Joens - Bert Nash WRAP (Lawrence)
Andrea Kerns - Children’s Mercy Hospital (Kansas City)
Lacie Koester - The Family Conservancy (Kansas City)
Pamela Leiker - Heart of Kansas Health Center (Great Bend)
Crystal Lindenman - High Plains Mental Health Center (Hays)
Flor Marquez - St. Francis Community Services (Garden City)
Marcia Mauch - Central Kansas Cooperative (Salina)
Conner McFarlin - Kansas City, Kansas Schools (Kansas City)
Sharee Smallwood - Children’s Mercy Hospital (Kansas City)
Carlos Rivera - Dodge City Schools (Dodge City)
Monica Rojas - Compass Behavioral Health (Dodge City)
Vanessa Roybal - Compass Behavioral Health (Garden City)
Jason Southard - Marillac (Overland Park)
Azure Sitting Up Stapleton - Bert Nash WRAP (Lawrence)
Emily Stortenbecker - PACES (Kansas City)
Meghan Suman - Johnson County Mental Health Center (Olathe)
Rachel Swenson - Southwest Guidance Center (Liberal)
Stephanie Taylor - Marillac (Overland Park)
RayeAnn Underwood - Bert Nash Health Connections (Lawrence)
Leah Womelsdorf - Ashby House (Salina)
Behavioral Health Workforce Development
Increased Supply of Social Workers
- Since 2016, the Scholars Program has graduated 305 new MSWs
- The program has provided over $3 million in scholarship support
- Scholar graduates include 118 persons of color and 52 bilingual individuals
- Around 62% had a rural background (lived in a rural area at some time)
- The majority of graduates are employed in Kansas including the KC metro area with around a third working in rural communities
- Graduates are employed by FQHCs, CCBHC/CMHCs, schools, hospital/health systems, child development services and substance use treatment facilities among other organizations
Integrated Health Scholars Program Graduates 2016-2023 Location of Employment (indicated in red) on Kansas Health Professional Shortage Area for Mental Health map (KDHE). Darker green/larger numbers indicate greater need.
In addition to the graduates working in Kansas, a number of graduates work in other states or they are currently on leave, disability, or retired.
Adding to the Knowledge
The Scholars Program conducts evaluation and research to understand and promote effective practices in behavioral health recruitment, retention and training. Our recent publications and presentations are featured below.
Publications & Presentations
Buller, C., Levy, M., Matejkowski, J., Carr, K., Busenhart, C.A., Peterson, J. & Paramesh, C. (2023). In-person and virtual delivery of a multigenerational, unfolding case study to support student learning and skill development in interprofessional collaboration. Journal of Interprofessional Education & Practice, 31.
Levy, M. & Boyd, C. (2021). Grow your own: Educating social workers in rural and frontier areas to address the behavioral health workforce crisis.Contemporary Rural Social Work Journal,13(1), Article 1.
Robertson, A. D., Crowl, A. N., Matejkowski, J., Levy, M., Boyd, C., Barnes, J., & S Shrader. (2021). Use of a warm handoff interprofessional simulation to model asynchronous and patient-centered teamwork. Journal of Interprofessional Education & Practice, 22(1000410).
Acquavita, S., Lee, B., Levy, M., Holmes, C., Sacco, P. & Harley, D. (2020). Preparing Master of Social Work students for interprofessional practice. Journal of Evidence-based Social Work, 17(5), 611-623.
Crowl, A., Wellner, Z., Levy, M., Boyd, C., Bates, J., Barnes, J., & Shrader, S. (2020). Determining the impact of an interprofessional simulation focused on social determinants of health with pharmacy students. Currents in Pharmacy Teaching & Learning, 13(7).
Holmes, C., Levy, M., & Boyd, C. (2017, August). Exploring social work preparation for integrated behavioral health care. University of Kansas School of Social Welfare.
Sacco, P., Johnson, S., Matejkowski, J., Levy, M. & Beaulieu, M. (2025, Oct 24). Long term impact of BHWET behavioral health fellowships: Data from three grantees. Council on Social Work Education’s 71st Annual Conference, Denver, Colorado.
Levy, M. (2025, Apr 16). Academic Partner Panel Presentation. Workforce Collaboration Forum. Community Care Network of Kansas. Panelist.
Boyd, C. & Levy, M. (2025, Apr 7). Building resilience and protective factors in the trauma workforce: Caring for those that care. 22nd Annual Hawai’i International Summit, Institute on Violence, Abuse and Trauma, Honolulu, Hawai’i.
Levy, M. (2025, Feb 4). Realistic job previews: A tool for health workforce recruitment & retention. Recruiting and Retaining the Rural Health Workforce. Rural Health Peer Learning Team Webinar. HRSA Health Center Program.
Levy, M. (2024, Dec 9). Integrated behavioral health workforce development. Workforce Roundtable. Community Care Network of Kansas.
Peterson, J. & Levy, M. (2024, Oct 10). Navigating the overlaps in social determinants of health. Building Healthy Communities 2024 ECHO: Patient Engagement and Social Determinants in Underserved Communities. University of Kansas Medical Center.
Levy, M. & Matejkowski, J. (2024, Jun 27). Increasing access to behavioral health through student training in telehealth and technology. 49th Annual National Institute on Social Work and Human Services in Rural Areas: On the Road to Thriving Rural Communities. Hays, Kansas.
Levy, M., Horton, A., & Goheen, L. (2024, May 31). Intro to the social work profession. Psychology Didactic Lecture, University of Kansas Medical Center.
Levy, M. & Matejkowski, J. (2023, Oct 27). Advancing health equity through improving access to behavioral health care. 2003 Kansas Health Equity Summit. Topeka, Kansas
Levy, M. & Matejkowski, J. (2023, Oct 1-4). Creating future social work leaders for integrated and remote health care. 58th Annual Meeting and Conference, Society for Social Work Leadership in Health Care, Atlanta, Georgia.
Levy, M. (2023, May 2). Increasing behavioral health access through a social work student training initiative. Webinar. Rural Health Council – Committee on Behavioral/Mental Health, University of Kansas Medical Center.
Levy, M. (2020, Sept 4). Providing behavioral health care in rural communities and with rural populations. Invited presenter, Psychology Didactic, University of Kansas Medical Center, Kansas City, KS.
Levy, M., Boyd, C. & Carr, K. (2019, Oct). Interprofessional education and social work: Preparing students and promoting the profession. Council on Social Work Education 65th Annual Program Meeting, Denver, CO.
Levy, M., Johnston, K., Randolph, S., Boyd, C. & Shrader, S. (2019, Sept). It takes a village: Growing a pipeline through innovation and collaboration. Invited presentation/panelist. 3RNet National Rural Recruitment and Retention Network, 2019 Annual Conference, Wichita KS.
Levy, M. (2019, April). Integrated Health Scholars Program. Navigating Rural Health Resources Webinar, Kansas Department of Health and Environment, Primary Care and Rural Health.
Levy, M. & Holmes, C. (2016, December). Preparing social work students for interprofessional practice in integrated health care. Academic Day Interprofessional Poster Session, University of Kansas Medical Center, Kansas City, Kansas.
Hunter, E., Renick, E., Paolo, T., Levy, M., Holmes, C., Matejkowski, J. (2017, November). An interprofessional collaboration between clinical psychology and clinical social work training programs that focuses on preparing students for practice and service to rural and urban underserved populations. Faculty Academic Day & Interprofessional Preceptor Summit, University of Kansas Medical Center, Kansas City, Kansas.
Levy, M., Holmes, C., & Boyd, C. (2017, September). Preparing the behavioral health workforce for integrated care in rural communities. Invited presenter at 2017 HRSA Virtual Behavioral Health Conference.
Levy, M., Holmes, C., & Boyd, C. (2017, March). Preparing master’s level social work graduates for integrated behavioral health. (2017, March). Invited plenary session, Sunflower Foundation Integrated Care Learning Collaborative, Topeka, KS.
Lee, B., Aquavita, S., & Levy, M. (2018). Preparing MSW students for interprofessional practice: Three programs share lessons learned. Council on Social Work Education 64th Annual Program Meeting, Orlando, Florida.
Wellner, Z., Crowl, A., Levy, M., Boyd, C., Bates, J., Barnes, J. & Shrader, S. (2018, November). Determining the impact of an interprofessional simulation focused on social determinants of health with pharmacy and social work students. Interprofessional Poster Session at Faculty Academic Day & Interprofessional Preceptor Summit, University of Kansas Medical Center, Kansas City, Kansas.
Levy, M. (2018, July). Educating social workers for health care practice. Invited presenter & discussion facilitator, Society for Social Work Leadership in Health Care, Mo-Kan Chapter, Mid-America Rehabilitation Hospital, Overland Park, Kansas.
Levy, M. (2018, April). Examining social determinants of health from rural and urban community perspectives. Invited presenter & panelist, Kansas Center for Cultural Competency Advancement, Webinar.